The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 26, Issue 2 / December 2022
Research Article Pages:101-106
10.5935/0946-5448.20220015
An Overview of the Effect of Age at Time of Cochlear Implantation on Language Outcomes in Jordan: A Retrospective Cohort Study.
Authors: Mohammad Al-Alawneh, Ra'ed al-Ashqar, Amjad Nuseir, Ahmad Al Omari, Mohammad kharisat, Firas Alzoubi
PDF
Abstract
Introduction: Cochlear Implantation (CI) surgery has long been used as an effective treatment for children with bilateral profound sensorineural hearing loss who failed to benefit from the use of hearing aids. Among other factors, the age at which implantation is done is thought to have an effect on the speech progression outcome of patients postoperatively.
Objectives: The Jordanian CI Program) has limited resources, and Jordan has an underdeveloped early screening and intervention program for deafness. In this study, we aimed to explore the effect of age at time of implantation on receptive and expressive language outcomes in Jordan, to guide funding and focus efforts on patient groups who would benefit most, thus reducing unnecessary longterm morbidity and disability, and improving cost efficiency
Methods: Data was gathered from all major sectors in Jordan on patients who underwent CI from 2006 to 2018 (a total of 1815 patients). We compared the language outcome 2 to 4 years after implantation for patients aged below 3 years, 3 to under 6, 6 to under 9 years, and 9 and older at the time of implantation
Results and Conclusion: We found a statistically significant difference in language outcomes between patients aged below 6 years vs those 6 and older, with better receptive and expressive language outcomes in the younger age groups.
Keywords: Tinnitus, cochlear implantation surgery.
Introduction
Cochlear Implantation (CI) has been widely recognized as a safe and effective procedure for the treatment of children with bilateral severe to profound sensorineural hearing loss, who have minimal to no improvement with the use of conventional hearing aids1. The goal of cochlear implantation is to improve the patients’ auditory perception, and hence, improve receptive and expressive language. However, as clarified in many studies, improved auditory perception and sound discrimination do not always translate to the ability to speak in a meaningful manner, as countless other factors affect language outcomes in patients2.
Factors such as compliance to external device use, age at time of cochlear implantation, socioeconomic status, access to specialized education and intervention programs, the presence of behavior disorders (ADHD, ASD), and the length of time spent using the device (implant experience). All play important roles in determining the overall language outcomes of CI patients3. In this study, we explored the effect of age at time of cochlear implantation (in years) on receptive and expressive language outcomes in Jordan, comparing outcomes for patients aged under 3 years at time of cochlear implantation, 3 years to 6 years, 6 years to 9 years, and 9 and older (up to age 20) at time of surgery, to determine the age group in which CI would be of most benefit, and thus guiding health sectors in improving population screening programs and early intervention programs, and directing financing to support patients in which surgery will be most beneficial, thus also improving cost efficiency.
Methods
This retrospective cohort study involved collecting data from the Jordanian ministry of health, Jordanian Royal Medical Services, and tertiary University hospitals in Jordan about patients who underwent cochlear implantation surgery from the year 2006 to the year 2018. Of these, we selected patients without missing data, who all had bilateral severe to profound SNHL preoperatively with the onset of hearing loss at age below 6 months, were all pre-lingual at time of surgery, with this surgery being their first CI, and all patients received a unilateral cochlear implant. All patients who were not compliant with external device use or had no access whatsoever to postoperative rehabilitation for any reason were excluded. Furthermore, patients with underlying behavioral disorders, post-operative complications, or incomplete electrode insertion were excluded.
Of the patients fitting these criteria, we divided them into 4 subgroups for comparison, patients aged below 3 years at time of implantation (320 patients), patients aged 3 to under 6 years (208), 6 to under 9 years (94), and from 9 to 20 years (51). 145 of the 528 patients aged below six years were also randomly selected for this study. All patients were implanted with devices from one of 2 companies, MED-EL and Cochlear. All patients were assessed 2 to 4 years after implantation by speech-language pathologists at one of 2 centers in Jordan, using a combination of the language screening test, listening progress profile test (LiP test), Meaningful Auditory Integration Scale (MAIS), and Infant Toddler MAIS (IT-MAIS) depending on patient age, as well as a subjective assessment of speech intelligibility. After a full assessment, they were given an overall score for expressive and receptive language outcomes of either poor, intermediate, good, or excellent. All patients were classified as poor preoperatively.
The relationship of the variable “age at time of cochlear implantation” to receptive and expressive language outcomes was analyzed using the Chi-squared test and fisher’s exact test where appropriate, with statistical significance concluded at P values of <0.05.
Results
Of the 1815 patients who underwent cochlear implantation from the year 2006 to 2018, after excluding the patients who did not fit our study criteria, we were left with 673 patients, 528 of these aged below 6 years (78.5%) and 145 aged between 6 and 20 years (21.5%) at time of implantation. We further subdivided these into 4 groups, patients aged younger than 3 years (320 patients), patients aged from 3 to under 6 years (208 patients), patients aged from 6 to under 9 (94), and those aged from 9 to 20 years (51).
The language progression scores were evaluated for all patient groups between 2 to 4 years post-implantation, and each patient was given a score of either poor, intermediate, good, or excellent. We then compared the speech progression outcomes of each age group with the older age group to determine if there was a significant difference in postoperative outcomes between patient groups.
When comparing patients aged under 3 years (320) with those aged 3 to under 6 years (208), we found there was no significant difference in the expressive and receptive language outcomes between the 2 age groups (P=0.420). Similarly, there was no statistically significant difference in the language outcomes post cochlear implantation between patients aged 6 to under 9 years and those aged 9 and older (P=0.114). Furthermore, analysis was done to compare the relationship between all 4 age groups and the receptive and expressive language outcomes, and statistical significance was found between age at time of implantation and language outcomes (P<0.00001).
Specifically, when comparing speech progression outcomes between patients aged 3 to under 6 years, and those aged 6 to under 9 years, we found there was a significantly better outcome in the younger age group (P<0.00001). This indicates that the turning point in our study for increased benefit with regards to language outcomes post-cochlear implantation is around 6 years of age. We, therefore, went on to analyze the difference overall between all patients aged under 6, and patients aged 6 and older. Data comparing language outcomes between all patient groups is summarized in Table 1.
| Speech Progression Status | 0 to 3 (320) | 3 to 6 (208) | 6 to 9 (94) | 9 to 20 (51) |
| Poor | 27 (8.4%) | 12 (5.8%) | 32 (34%) | 8 (15.7%) |
| Intermediate | 75 (23.4%) | 60 (28.8%) | 27 (28.7%) | 17 (33.3%) |
| Good | 88 (27.5%) | 56 (26.9%) | 21 (22.3%) | 17 (33.3%) |
| Excellent | 130 (40.6%) | 80 (38.5%) | 14 (15%) | 9 (17.7%) |
Table 1: Demonstrate speech progression and language outcomes according to the age of cochlear implantation in all groups.
A random sample of 145 patients was also selected from the 528 patients aged below six for comparison. Of these, 6.9% were given a score of poor compared to 27.6% of the group aged 6 and older, 29.7% were given a score of intermediate compared to 30.3%, 32.4% were given a score of good compared to 26.2%, and 31% given a score of excellent compared to 15.9% (Table 2).
| Speech Progression Status | Under 6 years (145 total) | 6 years and older (145 total) |
| Poor | 10 (6.9%) | 40 (27.6%) |
| Intermediate | 43 (29.7%) | 44 (30.3%) |
| Good | 47 (32.4%) | 38 (26.2%) |
| Excellent | 45 (31%) | 23 (15.9%) |
Table 2: comparing speech progression and language outcomes according to the age of cochlear implantation between a random sample of age group under 6 years and age group 6 years and older.
For easier comparison, we grouped the patients’ scores into 2 groups signifying significant improvement in expressive and receptive language outcomes vs subpar improvement, with Poor and Intermediate scores being grouped, and Good and Excellent together. In the younger age group, 36.6% had subpar outcomes post cochlear implantation compared to 58% of the older age group, and 63.4% were considered to have a good to excellent language outcome compared to 42% of the older age group (Table 3).
| Speech Progression Status | Under 6 years (145 total) | 6 years and older (145 total) |
| Poor/Intermediate | 53 (36.6%) | 84 (58%) |
| Good/Excellent | 92 (63.4%) | 61 (42%) |
Table 3: Comparing speech progression and language outcomes according to the age of cochlear implantation between a random sample of age group under 6 years and age group 6 years and older.
We found a statistically significant difference between the speech progression outcomes of the 2 age groups (P=0.0003), with better expressive and receptive language outcomes in patients below 6 years.
Similarly, we compared the older age group of 145 patients aged 6 years and older with all patients aged below 6 years (528 patients). Here we found that of the 528 patients, 7.4% scored Poor, 25.6% intermediate, 27.3% Good, and 39.8% Excellent. These ratios are similar to that of the random sample of 145 patients, showing that it is likely accurately representative of the whole sample (Table 4).
| Speech Progression Status | Under 6 years (528 total) | 6 years and older (145 total) |
| Poor | 39 (7.4%) | 40 (27.6%) |
| Intermediate | 135 (25.6%) | 44 (30.3%) |
| Good | 144 (27.3%) | 38 (26.2%) |
| Excellent | 210 (39.8%) | 23 (15.9%) |
When comparing all patients under 6 with those 6 and above, grouped into 2 categories as before, 33% of patients under 6 years had subpar scores compared to 58% of the older age group, and 67% had Good/Excellent scores compared to 42% of patients aged 6 and older (Table 5).
| Speech Progression Status | Under 6 years (528 total) | 6 years and older (145 total) |
| Poor/Intermediate | 174 (33%) | 84 (58%) |
| Good/Excellent | 354 (67%) | 61 (42%) |
Table 5: Comparing speech progression and language outcomes according to the age of cochlear implantation between ages under 6 years and age 6 years and older.
Analysis done on both these data sets again showed statistical significance between the 2 groups, with P<0.00001, further solidifying the difference between the speech progression outcomes of all patients aged below 6 and those aged 6 and above, with the younger age group showing significantly better expressive and receptive language outcomes than patients aged 6 years and older.
Discussion
Cochlear Implantation surgery is a relatively common procedure indicated in the treatment of bilateral severe to profound sensorineural hearing loss, with generally good results. It is mostly indicated in patients who do not improve with the use of conventional hearing aids. However, patients with pre-implant residual hearing have also shown improved speech recognition post cochlear implantation4,5 and there is ample evidence that adults with post-lingual deafness also show significant benefit from the use of cochlear implantation6.
The speech perception, receptive and expressive language outcomes post cochlear implantation are likely affected by many factors, such as patient compliance to external device use, implant experience, socioeconomic status, family and educational support, access to specialized education and rehabilitation centers, access to training with a speech and language pathologist, the presence of behavioral disorders, as well as anatomical abnormalities affecting surgery7-9.
In this study, we focused on studying the effect of age at time of implantation on expressive and receptive language outcomes. While many studies have shown that pre-lingual adolescents and adults with profound sensorineural hearing loss show significant improvement in speech perception post cochlear implantation10-13, it is well documented that implantation at a younger age leads to improved outcomes for patients14,15. Alsanosi et al. in a study done in Saudi Arabia, found that patients who were implanted below the age of 5 years had a better outcome in the form of better auditory skills, speech perception, and language production16. Similarly, Vishal Gaurav et al. in a study done in India, found that mean auditory perception outcomes (in the form of CAP and MAIS scores) in cochlear implant recipients were significantly better in patients operated below the age of 5 years compared to those over 5 years of age, although there was a clear benefit for patients aged above 5 years as well17.
The reason for this increased benefit from CI at a younger age is not fully understood, although it is thought that there is a critical period for development in the neural auditory pathway in the younger age group, and deprivation of auditory stimuli in this period may have longstanding effects on development, whereas, above the age of 5 to 6 years, there is relative plasticity in the auditory system18. However, a comparison of the effects of age at implantation with language outcomes may not be so simple, as other confounding factors can affect results. As age of implantation is reduced, the length of time using the device (implant experience) is increased. Furthermore, a comparison of outcomes is usually done over the same duration of use for older and younger patients, and so the age at testing varies, but cognitive and language development does not progress linearly with age. Therefore, our results in evaluating levels of progress may be affected by the different developmental levels at the time of evaluation18. As such, we must be cautious when interpreting our results.
In our study, we retrospectively reviewed the data from 1815 patients who underwent cochlear implantation surgery in Jordan (in all medical sectors) from the year 2006 to 2018. We selected all patients who had no missing data, had pre-lingual deafness with this surgery as their first CI, were compliant with external device use, underwent post-operative rehabilitation at any point, had no behavioral disorders, and had no surgical complications (673 patients). We further divided these patients into 4 groups for comparison, to determine the age group where cochlear implantation is of the most benefit. We divided them into patients aged under 3 years (320), patients aged from 3 to under 6 years (208), 6 to under 9 years (94), and 9 years and older (51).
Factors such as socioeconomic status, access to specialized education and family support, and the presence of anatomical abnormalities were not considered. All patients were evaluated 2 to 4 years after cochlear implantation by one of two centers in Jordan using a combination of LiP test, Language screening test, MAIS and IT-MAIS scores, and speech intelligibility assessment and were given an overall score for expressive and receptive language outcomes of Poor and Intermediate for subpar improvement, and Good and Excellent for significant improvement.
When comparing language outcomes between the different age groups, we found that there was no significant difference between patients aged under 3 years and those aged 3 to under 6 years at time of implantation. There was also no significance between the outcomes for patients aged 6 to under 9 years and those aged 9 and older. However, there was a significant relationship overall between age at time of implantation and receptive and expressive language outcomes.
More specifically, we found that there was a statistically better language outcome between patients aged 3 to under 6 years at time of implantation vs those aged from 6 to under 9 years. This clarified that, in our study group, the turning point in relation to age at time of implantation for the difference in benefit with regards to receptive and expressive language outcomes is around 6 years of age, in line with the studies mentioned previously, possibly owing to the increased plasticity of the auditory system around this age. Data on the comparison between the language outcomes between our patient groups are summarized in Figure 1.
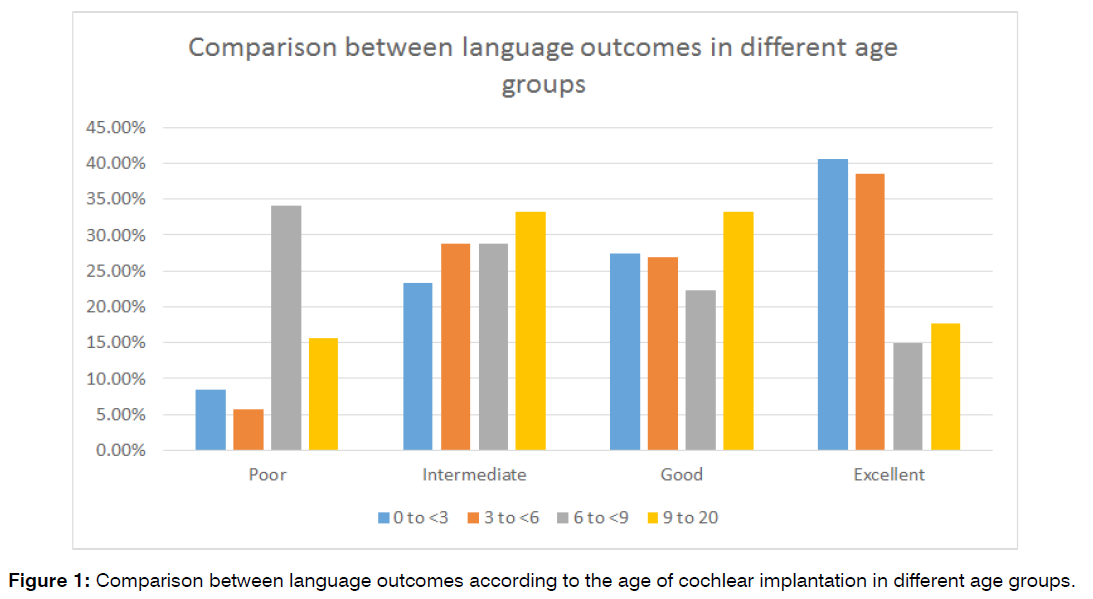
Figure 1: Comparison between language outcomes according to the age of cochlear implantation in different age groups.
We, therefore, went on to analyze the difference between all patients aged under 6 years vs those aged 6 and older to further clarify our results. When comparing all 528 patients aged below 6 with the 145 patients aged 6 and older, we found the younger age group had significantly better expressive and receptive language outcomes than the older age group, with 39.8% of the patients aged under 6 being scored excellent compared to 15.9% of those 6 and older, 27.3% scored Good compared to 26.2% of the older group, 25.6% scored intermediate compared to 30.3%, and only 7.4% scoring Poor compared to 27.6% of patients 6 and older. This data is summarized in Figure 2.
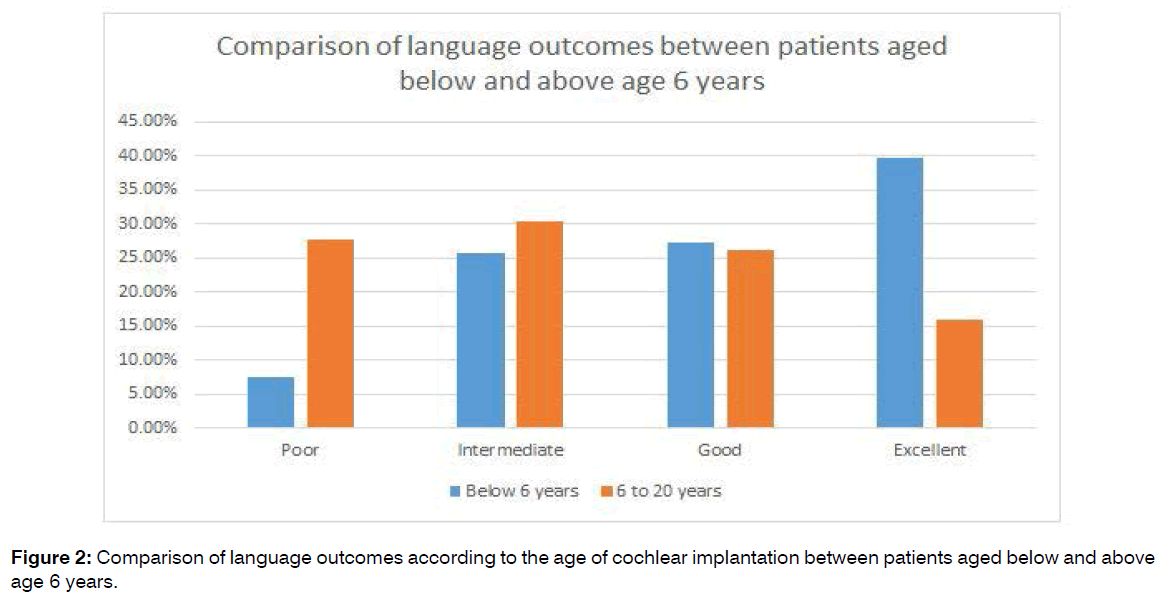
Figure 2: Comparison of language outcomes according to the age of cochlear implantation between patients aged below and above age 6 years.
To eliminate any bias, we randomly selected 145 patients of the 528 patients aged below 6 and compared them with the 145 patients aged 6 and older and found similar percentages of patients in each score as the total 528 patients, indicating the random sample is representative of the total patient group. For this group, we also found a statistically significant difference in the outcomes of the 2 groups, with significantly better expressive and receptive language outcomes in patients aged under 6 than those aged 6 and older. However, the data also shows a significant benefit to cochlear implantation in patients aged 6 years and older, even if not as clearly defined as that of the younger patients, with 42% showing significant improvement in receptive and expressive language outcomes post-implantation.
Conclusion
While many factors affect the expressive and receptive language outcomes of cochlear implantation surgery, when comparing the variable “age at time of cochlear implantation” to the language outcome, we found a significant difference between the younger age groups and the older, specifically differing at around the age of 6 years, showing that the earlier the implantation is done, the better the speech progression and language outcomes. While there is still a clear benefit in older patients, we hope this data helps guide population screening programs, early intervention programs, and in aiming for earlier diagnosis and intervention and focusing funding for early cochlear implantation surgery to achieve the best results possible for patients with early-onset deafness and improving cost efficiency.
References
- Szyfter W, Karlik M, Sekula A, Harris S, Gawecki W. Current indications for cochlear implantation in adults and children. Otolaryngologia Polska. 2019;73:1-5.
- Gaurav V, Sharma S, Singh S. Effects of age at cochlear implantation on auditory outcomes in cochlear implant recipient children. Indian J Otolaryngol and Head & Neck Surg. 2020;72(1):79-85.
- Holden LK, Firszt JB, Reeder RM, Uchanski RM, Dwyer NY, Holden TA. Factors affecting outcomes in cochlear implant recipients implanted with a perimodiolar electrode array located in scala tympani. Otol & neurotol: official publication of the Am Otological Soc, Am Neurotol Soci [and] Eur Academy of Otol and Neurotol. 2016;37(10):1662.
- Varadarajan VV, Sydlowski SA, Li MM, Anne S, Adunka OF. Evolving criteria for adult and pediatric cochlear implantation. Ear, Nose & Throat J. 2021;100(1):31-7.
- Fitzpatrick E, McCrae R, Schramm D. A retrospective study of cochlear implant outcomes in children with residual hearing. BMC Ear, Nose and Throat Disorders. 2006;6(1):1-6.
- Hamerschmidt R, Santos VM, Gonçalves FM, Delcenserie A, Champoux F, de Araujo CM, et al. Changes in cognitive performance after cochlear implantation in adults and older adults: a systematic review and meta-analysis. Int J Audiol. 2022:1-2.
- Cejas I, Hoffman MF, Quittner AL. Outcomes and benefits of pediatric cochlear implantation in children with additional disabilities: A review and report of family influences on outcomes. Pediatr Health, Med and Ther. 2015;6:45.
- Black J, Hickson L, Black B, Perry C. Prognostic indicators in paediatric cochlear implant surgery: a systematic literature review. Cochlear Implants Int. 2011;12(2):67-93.
- Silva JD, Yamada MO, Guedes EG, Moret AL. Factors influencing the quality of life of children with cochlear implants. Braz J Otorhinolaryngol. 2020;86:411-8.
- Wooi Teoh S, Pisoni DB, Miyamoto RT. Cochlear implantation in adults with prelingual deafness. Part I. Clinical results. The Laryngoscope. 2004;114(9):1536-40.
- Debruyne J, Janssen M, Brokx J. Late cochlear implantation in early-deafened adults: A detailed analysis of auditory and self-perceived benefits. Audiol and Neurotol. 2017;22:364-76.
- Craddock L, Cooper H, Riley A, Wright T. Cochlear implants for pre-lingually profoundly deaf adults. Cochlear Implants Int. 2016;17(sup1):26-30.
- Zeitler DM, Anwar A, Green JE, Babb JS, Friedmann DR, Roland JT, et al. Cochlear implantation in prelingually deafened adolescents. Arch of Pediatr & Adolescent Med. 2012;166(1):35-41.
- Robbins AM, Koch DB, Osberger MJ, Zimmerman-Phillips S, Kishon-Rabin L. Effect of age at cochlear implantation on auditory skill development in infants and toddlers. Arch of Otolaryngol–Head & Neck Surg. 2004;130(5):570-4.
- Nicholas JG, Geers AE. Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe to profound hearing loss. J Speech Lang Hear Res. 2007;50(4):1048-62.
- AlSanosi A, Hassan SM. The effect of age at cochlear implantation outcomes in Saudi children. Int J Pediatr Otorhinolaryngol. 2014;78(2):272-6.
- Gaurav V, Sharma S, Singh S. Effects of age at cochlear implantation on auditory outcomes in cochlear implant recipient children. Indian J Otolaryngol and Head & Neck Surg. 2020;72(1):79-85.
- Nicholas JG, Geers AE. Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe to profound hearing loss. J Speech Lang Hear Res. 2007;50(4):1048-62.
Department of Special Surgery, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan.
Send correspondence to:
Mohammad Al-Alawneh
Department of Special Surgery, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan. Tel no: 0092798531502, Email: Mialawneh@just.edu.jo
Paper submitted on September 21, 2022; and Accepted on October 19, 2022
Citation: Mohammad Al-Alawneh, Ra’ed Al-Ashqar, Amjad Nuseir, Ahmad Al Omari, Mohammad kharisat, Firas Alzoubi. An Overview of the Effect of Age at Time of Cochlear Implantation on Language Outcomes in Jordan: A Retrospective Cohort Study. Int Tinnitus J. 2022;26(2):101-106.


