The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 28, Issue 1 / June 2024
Research Article Pages:70-76
10.5935/0946-5448.20240013
Association between Anterior Cervical Osteophytes And Parasympathetic Dysfunction In Tinnitus Patients
Authors: Wim E. Tuinebreijer, Henk M. Koning*
PDF
Abstract
Background Tinnitus is a conscious perception of an auditory sensation in the absence of a corresponding external stimulus. Tinnitus can have a strong impact on the quality of life. The cause of tinnitus is not exactly known. Objectives To assess the reliability of portable infrared pupillometry. To study the hypothesis that enlarged anterior osteophytes of cervical vertebras influences the parasympathetic nervous system. Methods Nineteen tinnitus patients were examined with a portable infrared pupillometer and had X-ray examination of the cervical spine. The control patient population included 79 patients who visited the pain clinic for non-tinnitus complaints. Five different pupillometry values were estimated. The intraclass correlation coefficient was used to measure the inter-observer reliability. A multiple linear regression model was used to examine the association between the size of anterior osteophytes of cervical vertebras and pupillometry measurements. Results Inter-observer reliability was excellent for baseline pupil diameter and maximum constriction amplitude (values>= 0.75), moderate to good for pupillary constriction rate and maximum constriction velocity (values 0.41 - 0.74) and poor for latency constriction. Baseline pupil diameter, maximum constriction amplitude and maximum constriction velocity were significant lower in tinnitus patients. Multiple linear regression showed a significant effect of the size of anterior osteophyte of the sixth and third cervical vertebra and the intervertebral disc space between the third and fourth cervical vertebra on maximum constriction amplitude of the pupillometry measurement. In tinnitus patients a significant effect was found of hearing loss of 8 kHz on maximum constriction amplitude. Conclusion Inter-observer reliability was excellent for pupil diameter and maximum constriction amplitude (values>= 0.75) measured with a pupillometer. Pupil diameter, maximum constriction amplitude and maximum constriction velocity were significant lower in tinnitus patients. These results indicate that the parasympathetic nervous system is impaired. Large anterior osteophytes on the sixth and third cervical vertebra had a significant effect on maximum constriction amplitude, which we interpreted as an effect on the autonomous nervous system by activating the glossopharyngeal and vagal nerves. Pupillometry is valuable diagnostic measurement for tinnitus patients.
Keywords: Pupil Light Reflex, Pupillary reactivity, Constriction velocity, Reliability, Tinnitus, Cervical spondylosis, vagal nerve, Glossopharyngeal nerve
Introduction
Tinnitus is the conscious perception of diverse types of sound which are not caused by external acoustic stimuli. Tinnitus is common in the population with a prevalence of 10% - 15% [1]. Tinnitus is associated with male gender, hearing loss of high-pitched sounds and cervical pain [2]. The level of suffering and the comorbidities can be quite different, but the disruption of the life of tinnitus patients can be extremely high. This tinnitus related mental stress has been associated to imbalance of the Autonomous Nervus System (ANS) [3-5]. There is a negative reciprocity between tinnitus distress and parasympathetic markers [6].
The Pupil Light Reflex (PLR) is recommended as clinical diagnostic tool for ANS dysfunction [7]. These pupil size measurements are called pupillometry and can be performed by a portable infrared pupillometer [8]. Different parameters of the PLR can be used as indicators for either sympathetic or parasympathetic modulation. Parasympathetic dysfunction occurs commonly after 50 years of age, with hearing impairment, and with cervical pain [7,9,10].
Our study aims to address the research gap between tinnitus and the imbalance of the ANS being it the sympathetic or parasympathetic system. This study was performed to assess the reliability of portable infrared pupillometry and investigated the hypothesis that enlarged anterior osteophytes of cervical vertebras influences the Parasympathetic Nervous System (PNS).
Materials and Methods
Design
An observational retrospective study in Pain Clinic De Bilt, De Bilt, the Netherlands.
Ethical approval
The Ethics Committee United (Nieuwegein, the Netherlands) permitted this study (W24.062, March 27th, 2024). Each patient gave informed permission to the procedure.
Subjects
This study includes all patients subjected to pupillometry in Pain Clinic De Bilt between October 2023 and January 2024 (n = 98). The pupillometer was applied in all patients to both eyes. Patients with tinnitus or cervical pain had X-ray examination of the cervical spine. Patients with tinnitus underwent a two-sided audiogram for the tone thresholds from 250 to 8000 Hz (in dB hearing loss).
Data assessment
Obtained information included gender, age, length, body weight, body mass index (BMI), tinnitus features from the clinical questionnaire (dominant side of tinnitus, period of tinnitus, presence of diminished hearing, dizziness or balance disorders), measurements of the radiographs of the cervical spine, and serial measurements with quantitative pupillometry.
Radiograph of the neck
Measurements of the radiographs of the cervical spine are described in (Figure 1).
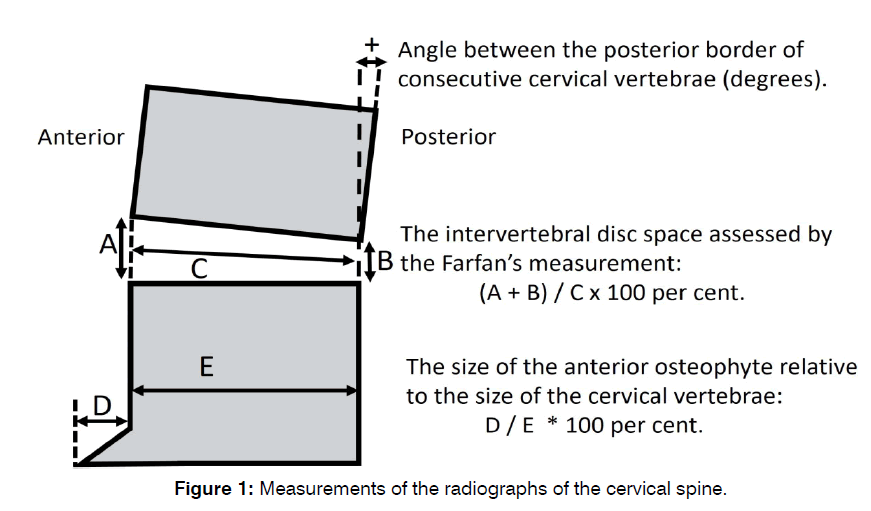
Figure 1: Measurements of the radiographs of the cervical spine.
Quantitative Pupillometry
Serial measurements with quantitative pupillometry were executed by two operators using an automated pupillometer (NeuroLight Algiscan, ID-MED, Marseille, France). The device contains a colour liquid crystal display screen, an integral illumination source, and an infrared camera capable of recording variation at the pupillary surface at 67 frames per second. A detachable rubber cup ensures accurate position and distance from the pupil. This adapter also encompasses the patient's orbit, placing the eye in the dark, preventing stray light and variation of light intensity between the measurements of the pupils. The pupillometer illuminates the eye with a calibrated light stimulus (320 Lux, 1 second). All data are recorded digitally, leading to accurate and objective assessments. Two assessments were executed for each eye of the patient. A minimum duration of five minutes was allowed between appraisals of the same pupil to obtain full recovery of baseline pupil diameter after light stimulation. The following observations were performed: baseline pupil size (mm), Latency of Constriction (LC) (msec), pupillary constriction rate (i.e., the difference between baseline and post-stimulation pupil size, expressed as % of constriction from the baseline value) (PCR), Maximum Constriction Amplitude (MCA) (mm), and Maximal Constriction Velocity (MCV) (mm/sec).
Statistics
Statistical analysis was performed using IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. The intraclass correlation coefficient with 95% confidence intervals was used to compute the inter-observer reliability. As a measure of test-retest agreement for each measure of pupillometry the standard error of measurement was calculated. Using the standard error of measurements the minimal detectable changes of the five pupillometry measures were calculated. Mean pupillometry values between patients with and without tinnitus were compared using unpaired t-tests. Multiple linear regression analyzed the relationship between MCA and several independent variables. Logistic regression was caried out to study the correlation between tinnitus and several predictors. Path analysis was performed using Amos (Version 24.0), Chicago: IBM SPSS to assess a tinnitus model.
Results
In the period from October 2023 to January 2024, there were 98 patients subjected to pupillometry in our clinic. The details of the patients are specified in (Table 1). There were more females than males.
| Characteristics | Number of patients | % | Mean | SD |
|---|---|---|---|---|
| Male | 40 | 41 | ||
| Female | 58 | 59 | ||
| Age (years) | 57 | 15 | ||
| Body Mass Index (BMI) | 28 | 12.3 | ||
| Tinnitus | 19 | 19.4 | ||
| Baseline pupil diameter (mm) | 3.9 | 0.88 | ||
| Maximum constriction amplitude (MCA) (mm) | 1.2 | 0.52 | ||
| Pupillary constriction rate (PCR) (%) | 30.7 | 8.94 | ||
| Maximum constriction velocity (MVC) (mm/sec) | 3.5 | 1.34 | ||
| Latency constriction (LC) (msec) | 241 | 52.6 | ||
Table 1: Patient characteristics and pupillometry values
In (Table 2) measures for reliability are presented which were calculated from repeated measurements of pupillometry. Reliability refers to the reproducibility of a measurement. The Intraclass Correlation Coefficient (ICC) indicates the inter-observer reliability. A two-way random-effect model and absolute agreement was selected. The measurements of baseline pupil diameter, the MCA, the PCR, and the MCV showed good inter-observer reliability, but the LC does not. The Standard Error of Measurement (SEM) and Minimal Detectable Change (MDC) or Smallest Detectable Change (SDC) for baseline pupil diameter, MCA and MVC was low and for PCR and LC high.
| Pupillometry | N | ICC | CI (95%) | SEM | MDC |
|---|---|---|---|---|---|
| Baseline pupil diameter (mm) | 158 | 0.91 | 0.85 - 0.94 | 0.67 | 1.85 |
| MCA (mm) | 158 | 0.8 | 0.73 - 0.85 | 0.21 | 0.59 |
| PCR (%) | 158 | 0.68 | 0.58 - 0.75 | 54.68 | 151.57 |
| MVC (mm/sec) | 158 | 0.71 | 0.62 - 0.78 | 1.63 | 4.51 |
| LC (msec) | 156 | 0.36 | 0.21 - 0.49 | 1376.91 | 3816.61 |
Table 2: Interrater reliability of measurements of pupillometry
Tinnitus started at the mean age of 47.1 years (min 27.0, max 74.0, SD 15.8). Tinnitus was in 33% one sided, 39% of the tinnitus patients showed balance complains, 33% complained of dizziness, 72% showed hearing loss, 78% complained of neck pain. Hearing loss was of high-pitched sounds (4-8 kHz) Mean pupillometry values between patients with and without tinnitus were compared using unpaired t-tests and are given in (Table 3). Significant lower values were seen in tinnitus patients for baseline pupil diameter, MCA, and MVC. The association between MCA and the size of anterior osteophytes, intervertebral disc spaces and angles between the posterior border of consecutive vertebrae, sex, age, and BMI was assessed using multiple regressions. Non-significant variables were pulled out one by one removing the largest P value first, until all remaining variables in the model were significant. The results are given in (Table 4).
| Tinnitus (N=38) | No tinnitus (N=158) | Difference (95% CI) | P value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Baseline pupil diameter (mm) | 3.52 (0.81) | 4.05 (0.86) | 0.53 (0.23 to 0.83) | 0.001 |
| MCA (mm) | 1.06 (0.50) | 1.29 (0.52) | 0.22 (0.04 to 0.41) | 0.017 |
| PCR (%) | 29.46 (11.62) | 30.95 (8.19) | 1.49 (-1.69 to 4.68) | 0.357 |
| MVC (mm/sec) | 3.09 (1.51) | 3.57 (1.29) | 0.49 (0.01 to 0.96) | 0.045 |
| LC (msec) | 233.95 (98.53) | 241.74 (34.30) | 5.05 (-16.4 to 26.5) | 0.853 |
Table 3: Comparison of pupillometry in patients with tinnitus and those without tinnitus
| Variable | Coefficient | 95% CI | Overall P value |
|---|---|---|---|
| Tinnitus | -0.327 | -0.505, -0.148 | <0.001 |
| Size anterior osteophyte 6th cervical vertebra | -0.019 | -0.034, -0.005 | 0.009 |
| Size anterior osteophyte 3rd cervical vertebra | -0.025 | -0.038, -0.011 | <0.001 |
| Intervertebral disc space between the third and fourth cervical vertebra | -0.026 | -0.038, -0.013 | <0.001 |
| Age | -0.006 | -0.012, 0.00 | 0.062 |
Table 4: Multiple regressions showing effects of tinnitus, size of the anterior osteophyte on the sixth and on the third cervical vertebra, intervertebral disc space between the third and fourth cervical vertebra on maximum constriction amplitude (mm)
Because only in tinnitus patients hearing was assessed a multiple regression in tinnitus patients was performed. The relation between MCA and the size of anterior osteophytes, intervertebral disc spaces, angles between the posterior border of consecutive vertebrae, sex, age, BMI and hearing loss (dB) at 250 Hz, 500 Hz, 1 kHz, 2 kHz, 4 kHz , 6 kHz and 8 kHz was estimated using multiple regression. Non-significant variables were taken out one by one removing the largest P value first, until all remaining variables in the model were significant. The results are given in (Table 5).
| Variable | Coefficient | 95% CI | Overall P value |
|---|---|---|---|
| Age | -0.015 | -0.031 | 0.019 |
| Intervertebral disc space between the third and fourth cervical vertebra | -0.025 | -0.05 | 0.004 |
| Hearing loss at 8 kHz | -0.007 | -0.014 | 0.024 |
Table 5: Multiple regression showing effects of age, intervertebral disc space between the third and fourth cervical vertebra and hearing loss at 8 kHz on maximum constriction amplitude (mm) in tinnitus patients
Logistic regression showing the relation between tinnitus versus the combined effect of MCA (mm), sex and angle between the sixth and seventh vertebrae is given in (Table 6). Each odds ratio is adjusted for MCA (mm) and sex. The odds ratio of sex (reference category female) is 0.07 (95% CI 0.02, 0.22). Can choose reference category to be first or last. This model has a percentage correct of 75.4%.
| Variable | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Maximum constriction amplitude (mm) | 0.35 | 0.13, 0.98 | 0.045 |
| Sex (male) | 14.18 | 4.52, 44.46 | <0.001 |
| Angle between the 6th and 7th cervical vertebrae | 1.32 | 1.14, 1.53 | <0.001 |
Table 6: Adjusted odds ratios for effects of maximum constriction amplitude, sex, and angle between the 6th and 7th cervical vertebrae on tinnitus
The odds are the chance of a certain outcome divided by one minus that chance. The odds ratio is the odds in one group patients (for instance the odds of male patients) divided by the odds of the other group of patients (female patients). The odd of having tinnitus is 14.2 as large for male patients. The interpretation of the odds ratio of continuous outcomes is more difficult because it is the change of one unit of the outcome (for instance one mm of MCA or for instance one percent of intervertebral disc space).
In (Figure 2) path analysis showing the relationship between two dependent variables: MCA and tinnitus and four independent variables: size of the anterior osteophyte on the sixth cervical vertebra, intervertebral disc space between the third and fourth cervical vertebra, age and sex in a model. The model shows a good fit to the data with a non-significant chi-square value. The null hypothesis stating the model is correct can’t be rejected. The regression weights of size of the anterior osteophyte on the sixth cervical vertebra, intervertebral disc space between the third and fourth cervical vertebra, and age are negative and decrease the value of MCA. The results on the variables show the mean and variance estimates and the covariances between the variables. Error variables with variance estimates and standard errors are attached to the two independent variables.
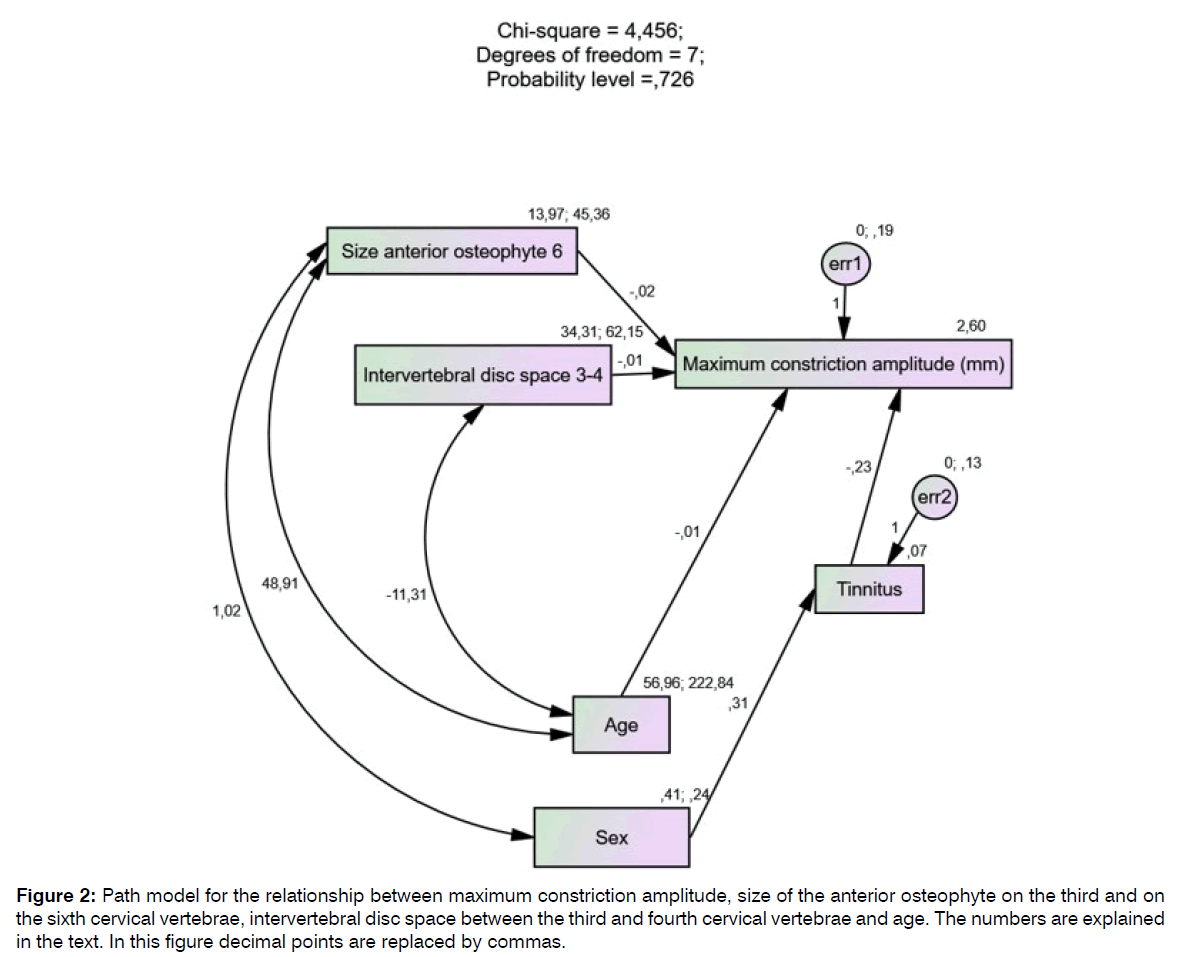
Figure 2: Path model for the relationship between maximum constriction amplitude, size of the anterior osteophyte on the third and on the sixth cervical vertebrae, intervertebral disc space between the third and fourth cervical vertebrae and age. The numbers are explained in the text. In this figure decimal points are replaced by commas.
Discussion
In this study we examined the use of a portable infrared pupillometer in a sample of nineteen patients with tinnitus. These patients were compared with 79 patients who also attended the Department of Pain. Five different pupillometry values were estimated. To our knowledge no studies have published data on the use of pupillometry in tinnitus patients. In accordance with the literature most of the tinnitus patients complained of hearing loss of high-pitched sounds (72%), cervical pain (78%) and the tinnitus was most often two-sided (67%) [2].
Inter-observer reliability was excellent for baseline pupil diameter and MCA (values>= 0.75), moderate to good for PCR and MVC (values 0.41 - 0.74) and poor for LC. For this reason, we advise to use the baseline pupil diameter and MCA as measures for pupillometry. The Standard Error of Measurement (SEM) is a parameter of measurement error and tells how far apart the two repeated measurements are. For baseline pupil diameter, MCA and MVC the two repeated measures were not far apart. But for the PCR and LC the SEM was high. The Minimal Detectable Change (MDC) or Smallest Detectable Change (SDC) is a change beyond measurement error (SEM) and was for baseline pupil diameter, MCA and MVC low and for PCR and LC high. The SEM, MDC and SDC are expressed in the unit of measurement of pupillometry.
Baseline pupil diameter, MCA and MVC were significant lower in tinnitus patients. These results indicate an impaired PNS 7. The PCR and LC were not different between patients with and without tinnitus. Multiple linear regression showed the effect of tinnitus and the size of the anterior osteophyte on the third and on the sixth cervical vertebra, intervertebral disc space between the third and fourth cervical vertebra, and age on MCA of the pupillometry measurement. This model without the size of the anterior osteophyte of the third cervical vertebra was confirmed in path analysis. All dependent variables in the model had a negative effect on MCA. Patients with tinnitus, older age, a large size of the anterior osteophyte of the sixth cervical vertebra and a large intervertebral space between the third and fourth cervical vertebra had a decrease of MCA of the pupillometry measurement.
In tinnitus patients a multiple linear regression presented a significant effect of hearing loss of 8 kHz on MCA. The association between the decrease of MCA of the pupillometry measurement and hearing loss at 8 kHz in tinnitus patients can be a cholinergic effect on the ANS by the parasympathetic nerves [11].
Logistic regression showed the relationship between tinnitus and the combined effect of MCA (mm), sex, angle between the 6th and 7th cervical vertebrae. Tinnitus lowers the effect of the MCA, male patients show more tinnitus, patients with an increased angle between the 6th and 7th cervical vertebrae show more tinnitus. The results do not imply causality since this is an observational study. Patients with tinnitus have a lower MCA but we believe that this correlation is caused by large size anterior osteophytes of cervical vertebrae.
The pupil size depends on the interplay between antagonistic actions of the circular sphincter pupillae muscle of the iris, innervated by the PNS, and of the radial dilator pupillae muscle, innervated by the sympathetic nervous systems [12]. The baseline pupil diameter is mainly controlled by sympathetic activity. In our study, significant lower values for baseline pupil diameter were found in tinnitus patients. This may indicate higher sympathetic activity in the non-tinnitus pain patients or lower sympathetic activity in the tinnitus patients. Efferent sympathetic pathways originate from the hypothalamus and travel via the pons and the lateral reticular medulla to the intermediolateral column of the cervico-thoracic spinal cord (segments C8-T2) [13]. The efferent sympathetic fibers project via the Superior Cervical Ganglion (SCG) to the radial dilatator pupillae muscle of the eye [12,14]. In the current study, there was no pupil dilatation in patients with tinnitus and therefore no signs of hyperactivity of the sympathetic nervous system.
The Edinger–Westphal Nucleus (EWN) within the oculomotor complex contains the pre-ganglionic parasympathetic neurons that control the iris sphincter [7]. The MCV and MCA parameters are regarded as the most sensitive markers of parasympathetic cholinergic activity [7,12]. The current results indicate impaired parasympathetic activity in tinnitus patients. A decrease in parasympathetic activity have been reported for a wide range of disorders, including tinnitus, aging, cervical spondylosis and hearing loss [3,7,10,14]. In chronic tinnitus patients, there is a negative correlation between tinnitus distress and parasympathetic markers [6]. In the currents study, multivariate analysis of the relationship between MCA and the measurements of the radiographs of the cervical spine, sex, age, and BMI indicated that large anterior osteophytes on the 3rd and 6th cervical vertebra had a significant effect on MCA. We concluded that enlarged anterior osteophytes of cervical vertebras impairs the PNS in tinnitus patients.
The locus coeruleus (LOC) plays a pivotal role in the pupil light reflex with excitatory projections to the intermediolateral cell column of the spinal cord, and inhibitory projection to the EWN [14]. Activation of the LOC produces an increase in sympathetic activity and a decrease in parasympathetic activity via these projections [15]. Hyperactivity of the LOC can explain our findings during pupillometry of tinnitus patients [15,16]. It receives afferents from multiple brain nuclei including the nociceptive collaterals of the spinothalamic tract, the hypothalamus, the central nucleus of the amygdala, the nucleus of the solitary tract (NTS), the nucleus paragigantocellularis and the nucleus prepositus hypoglossi [15-17]. The relay between the NTS and the LOC is conducted through two pathways: an excitatory pathway (via the nucleus paragigantocellularis in the rostral ventrolateral medulla) and an inhibitory pathway (via the nucleus prepositus hypoglossi). The nucleus paragigantocellularis provides the main excitatory inputs to the LOC. It receives inputs from the NTS and from primary afferent fibers of the glossopharyngeal and vagal nerves [18].
The effect of the large anterior osteophytes of cervical vertebrae is directly on the ANS by the parasympathetic nerves [7,16]. There is a close relation between the SCG and the vagal and glossopharyngeal nerves [19]. SCG fibers connect to the glossopharyngeal nerve at the upper region of the SCG and to the vagal nerve at the middle region of the SCG. Pathology in front of the cervical spine can activate the vagal and glossopharyngeal nerves leading to hyperfunction of the LOC and to a dysfunction of the PNS (Figure 3).
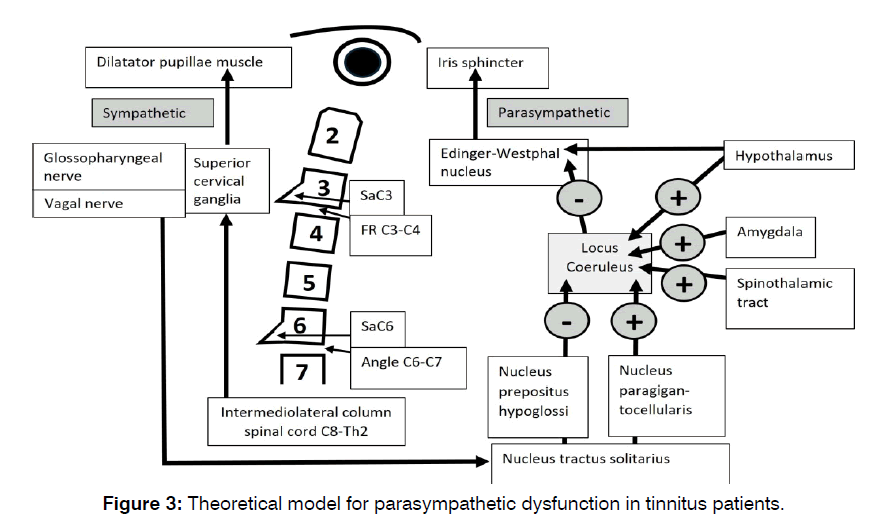
Figure 3: Theoretical model for parasympathetic dysfunction in tinnitus patients.
Conclusion
Pupillometry is valuable diagnostic measurement in tinnitus patients. We advise to use the baseline pupil diameter and MCA as measures for pupillometry. Baseline pupil diameter, MCA and MCV were significant lower in tinnitus patients. Large anterior osteophytes on the 3rd and 6th vertebra had a significant effect on MCA, which we interpreted as an effect on the ANS by activating the glossopharyngeal and vagal nerves. Pathology in front of the cervical spine can activate the vagal and glossopharyngeal nerves leading to hyperfunction of the LOC and to a dysfunction of the PNS. Treatment with cervical injections should be aimed on nerves along large anterior osteophytes of the cervical vertebrae.
Limitations
Small sample size was the major limitation of this study. Future studies will be necessary to evaluate the effect of tinnitus treatment on baseline pupil diameter and MCA.
References
- Schoisswohl S, Langguth B, Schecklmann M, Bernal-Robledano A, Boecking B, Cederroth CR, et al. Unification of Treatments and Interventions for Tinnitus Patients (UNITI): a study protocol for a multi-center randomized clinical trial. Clin Trials J. 2021;22:1-6.
- Koning HM, Ter Meulen BC. Pain in relationship to Tinnitus and Hearing Loss. Int Tinnitus J. 2021;25(2):124-8.
- Kaya H, Suner A, Koparal M, Yucetas SC, Kafadar S. Evaluation of Tp-e interval, Tp-e/QT ratio and index of cardiac-electrophysiological balance in patients with tinnitus. BMC Cardiovasc. 2021;21(1):415.
- Savov A. Tinnitus, heart rate variability, and some biochemical indicators. Int Tinnitus J. 1999;5:20-23.
- Miyoshi S, Eng M, Uemi N, Eng D, Ifukube T. Increased Parasympathetic Nerve Tone in Tinnitus Patients Following Electrical Promontory Stimu-lation. Int Tinnitus J. 1996;2(1):67-71.
- Van Der Loo E, Congedo M, Vanneste S, Van De Heyning P, De Ridder D. Insular lateralization in tinnitus distress. Auton Neurosci. 2011;165(2):191-4.
- Wang Y, Zekveld AA, Naylor G, Ohlenforst B, Jansma EP, Lorens A, et al. Parasympathetic nervous system dysfunction, as identified by pupil light reflex, and its possible connection to hearing impairment. PLoS One. 2016;11(4):e0153566.
- Larson MD, Behrends M. Portable infrared pupillometry: a review. Anesth Analg. 2015;120(6):1242-53.
- Arnold AC, Ng J, Lei L, Raj SR. Autonomic dysfunction in cardiology: pathophysiology, investigation, and management. Can J Cardiol. 2017;33(12):1524-34.
- Johnston RJ. Vertebrogenic autonomic dysfunction—subjective symptons: a prospective study. JCCA. 1981;25(2):51-7.
- Ruan Q, Yu Z, Zhang W, Ruan J, Liu C, Zhang R. Cholinergic hypofunction in presbycusis-related tinnitus with cognitive function impairment: emerging hypotheses. Front aging neurosci. 2018;10:98.
- Ferencová N, Višnovcová Z, Bona Olexová L, Tonhajzerová I. Eye pupil - a window into central autonomic regulation via emotional/cognitive processing. Physiol Res. 2021;70(4):S669-S682.
- Ziemssen T, Siepmann T. The investigation of the cardiovascular and sudomotor autonomic nervous system—a review. Front Neurol. 2019;10:436003.
- Wu F, Zhao Y, Zhang H. Ocular autonomic nervous system: An update from anatomy to physiological functions. J Vis. 2022;6(1):6.
- Suarez-Roca H, Mamoun N, Sigurdson MI, Maixner W. Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Compr Physiol. 2021;11(2):1373.
- Hall CA, Chilcott RP. Eyeing up the future of the pupillary light reflex in neurodiagnostics. Diagn Pathol. 2018;8(1):19.
- Szabadi E. Functional organization of the sympathetic pathways controlling the pupil: light-inhibited and light-stimulated pathways. Front Neurol. 2018;9:419676.
- De Cicco V, Tramonti Fantozzi MP, Cataldo E, Barresi M, Bruschini L, Faraguna U, et al. Trigeminal, visceral and vestibular inputs may improve cognitive functions by acting through the locus coeruleus and the ascending reticular activating system: a new hypothesis. Front Neurol. 2018;11:287938.
- Mitsuoka K, Kikutani T, Sato I. Morphological relationship between the superior cervical ganglion and cervical nerves in Japanese cadaver donors. Brain Behav. 2017;7(2):e00619.
1Trauma Research Unit, Department of Surgery,, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands
2Department of Pain therapy, Pain Clinic De Bilt, De Bilt, The Netherlands
Send correspondence to:
Henk M. Koning
Department of Pain therapy, Pain Clinic De Bilt, De Bilt, The Netherlands, E-mail: hmkoning@pijnkliniekdebilt.nl
Paper submitted on April 25, 2024; and Accepted on May 03, 2024
Citation: Henk M. Koning. Association between Anterior Cervical Osteophytes and Parasympathetic Dysfunction in Tinnitus Patients. Int Tinnitus J. 2024;28(1):070-076.


