The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:125-134
10.5935/0946-5448.20230020
Challenges Faced by Individuals with Hearing Impairment during COVID-19 Pandemic Lockdown â?? A Pilot Study
Authors: Abhilash Ghadei, Archita Kumari, Suresh Thontadarya, A. Srividya
PDF
Abstract
COVID – 19 (Corona Virus Infectious Disease) situations reported in 2019, declared by World Health Organization (WHO) as a pandemic is still a prevailing global crisis. Common regulations were implemented such as lockdown, wearing face masks as mandatory, face shields, gloves and maintaining physical and social distance in public places to reduce the spread of the virus. These pandemic induced challenges affected social communication, technical and behavioral aspects in lifestyle of people with hearing impairment. Along with medical, paramedical services, the crisis had challenged hearing, speech language pathology and therapy services too. The study aimed to explore the challenges that adults with hearing impairment had experienced during the pandemic and to suggest some practical solutions that can be implemented by audiologists. It is a questionnaire-based study with purposive sampling method employed in data collection. The questionnaire was administered on adult hearing aid users (mean age: 18 years) recruited for participation from different parts/ clinical setups across India. The outcome of the questionnaire did support the assumption that availing audiological services was difficult or impossible for most of the hearing aid users. Accessing batteries was reported to be the most frequent issue. Adequate level of hearing though hearing aid was important to them and clinical services could not be availed for long period of time due to travel related issues and closure of audiological services. Also, social isolation impacted on their quality of life and effective communication. As a possible solution most of the users chose tele services as a better solution.
Keywords: COVID-19, Hearing aid users, Challenges, Tele audiological services, Lockdown.
Introduction
COVID-19, an infectious disease caused by corona virus spread worldwide, caused dramatic changes in people’s overall lifestyle including delivery of healthcare services. Due to the severity of the spread, focus was on the funds, regulations, treatment protocol and prevention of its further spread. The inevitable regulations during the pandemic included using personal protection equipment such as face masks, face shields, and gloves as well as social and physical distancing. Government of India declared lockdown and imposed restrictions of international travel. The market areas, offices, schools, universities, airports, and large gatherings continued to be restricted to ensure public safety and control of COVID-19 transmission, as per the guidelines of the centers of pandemic control in India [1-3].
Providing clinical services during lockdown was difficult for premedical professionals such as audiologists, speech language pathologists, psychotherapists [4]. The guidelines were strictly against physical contact and social distancing; this challenged an audiologist as physical contact is required for providing audiological services. When the proximity of the testee from the tester, the duration of appointments and test setting is considered, the Centers for Disease Control and Prevention (CDC) recommended that audiological services represent a medium to high risk of COVID-19 infection [5]. The majority of individuals who need audiology services (>65 years old) are also at high risk of COVID19-related mortality and morbidity, hence, their health was prioritized over their hearing concerns.
Audiological treatment involves a high-touch service, requiring numerous face-to-face sessions in soundtreated environments for hearing assessments, hearing aid fittings, follow-up troubleshooting, and counselling. This usual audiological care pathway is currently unworkable due to the unexpected demand for physical distance and even long-term lockdown suggestions for older persons [2]. Considering the above-mentioned factors most of the clinical setups were nonfunctional during the period of lockdown and audiologists did not work as they do not come under emergency health workers and Speech and hearing centers are nonfunctional or provided limited services during this time period which made it difficult for individuals with hearing impairment in different age groups to avail proper rehabilitation. Along with the difficulties already mentioned, geriatric and adult hearing aid users have had trouble gaining access to technical assistance for their implants, accessory devices, and hearing aids, which are essential to assist people with hearing loss, regain their communication skills [1].
During lockdown due to limited services many practical issues arose affecting the quality of life in hearing aid users, such as lack of batteries, hearing aid servicing, hearing aid and fine tuning. Functioning of clinics and service centers were limited during the pandemic so availability of hearing aid battery was also difficult, mostly the problems occurred for non-rechargeable hearing aid users [3]. Users
of hearing aids frequently require support or monitoring from hearing healthcare professionals, especially in the case of geriatrics. However, this age group was at high risk for COVID-19 [6, 7]. During lockdown, availability of technical services such as fine tuning of hearing aids or changing gain of device were maximally affected for the users. Availability of different accessories related services such as changing ear moulds, ear tips, huggie and dry kit were also difficult for them. Even in case of new hearing aid fitting or hearing aid purchasing difficulty was raised during the lockdown3. Hearing loss affects hearing impairment in various ways, both directly and indirectly, and has a variety of communicative implications [5]. In addition, most governments have concentrated on reducing COVID-19- related mortality by implementing the world’s most upto- date treatment procedure and preventing the virus spread. Some regulations have been inevitably executed to fight against COVID-19. Personal protection items such as face masks, gloved and face shields, as well as social and distancing techniques, were some of them. In some countries, wearing a face mask in public locations is also required to prevent the infection from spreading. Although wearing a face mask is an unavoidable part of fighting the COVID-19 outbreak, it appears to have created some interaction and communication issues for individuals with hearing loss. Other than direct impact of hearing loss a list of associated problems also affected their qualityof- life style. For people with any degree of hearing loss, the repercussions of hearing loss led to inadequate communication. Communication difficulties caused by hearing loss affect social relationships in children and adolescents, leading to a variety of consequences such as major educational problems, psychological disorders such as depression, isolation, hopelessness, disappointment and in more severe cases aggression, as well as disruption of language and speech acquisition in younger children.
Tele clinical services are an optimal solution for availing services by the users but the implementation of the delivery system is in its infancy. In Tele mode of audiological services such as assessment and management are provided from a distance [8-10], which is an alternative to the direct or in person mode of services. This virtual mode of services can be offered in two ways: first, synchronously, with real-time videoconferencing, and second, utilizing the “store-and-forward” method, with information prerecorded, saved, and then transferred to a remote site [11, 12]. Tele-audiology can be used to do almost all part of audiology, including hearing screening, diagnosis, amplification device fitting and verification, and cochlear implant programming. The level of acceptance and attitudes of the hearing aid users towards tele audiological services also needs to be explored.
During this COVID-19, even after release from lockdown, it was advised that everyone, especially older adults were asked to stay at home since they were at greater risk. Although the pandemic had affected everyone, hearing aid users faced considerable challenges, particularly when there is limited functioning of audiological clinics. A study was done on effect of COVID-19 on Cochlear Implant Users and fond that lockdown affected the CI users [13] in several ways such as continuing AVT was difficult due to nonfunctioning of clinics, he also explored getting technical supports and other accessories was a bigger issue during this lockdown period. Especially when it comes to Indian perspective, the practical challenges reported by hearing aid users’ needs to be explored more in India. Compare to other rehabilitative services, the studies exploring challenges faced by hearing aid user in audiological perspective in India is very limited, hence the need for the study, which will be helpful to identify the problems such as limited availability of audiological services and problems in availability of batteries and accessories [14].
The study was aimed to understand the obstacles faced by hearing aid users during the COVID-19 outbreak. To achieve this, the data was collected in the form of questionnaire from the participants, and the results of the responses were analyzed. Before administration of the questionnaire, the participants were provided details of the test along with patient information sheet and informed consent was obtained.
Method
Participants: The data was collected in the period between 20 September 2021 and 26 October 2021, and the study included 31 hearing aid users above 18 years of age who had been using hearing devices for minimum of three months or more. [The use of hearing aid for minimum of three months is adequate for the person with hearing loss to understand the changes in their lives; also, this time period allows them to learn to operate their hearing aids appropriately] [15].
The sampling method followed for the study was purposive convenient sampling. This study aimed to recruit a variety of hearing aid users across different states of India in a short time. The data collection process started by involving of small set of participants from different clinical setups across India. Consent from all the participants was taken prior to the study. There were no ethical issues for the current study. Approval was taken from the ethical committee of the Institution. The ethical clearance certificate (Bshrf/RC/IEC/IM/12/2022) has been attached in the appendix section.
Inclusion and Exclusion Criteria: The participants recruited for the current study should be of more than 18 years. The participant should have been using hearing aid at least for 3 months. The participant should have fair level of understanding in English language which was confirmed through their demographic details and educational history. Should have previous audiological evaluation report. Individual should have fair level of cognition. Clients without their audiological evaluation report were not included in the study.
Individual who presented with obvious/reported, cognitive/ communicative impairment were not be included for the study. Hearing impaired population associated with high medical dependency, those who have moderate–severe levels of cognitive impairment as indicated within their medical history, with any severe motor dysfunction, dexterity issue, musculoskeletal issues were not be included and anyone with significant auditory or visual impairments were excluded.
Study Tool: For the study, a questionnaire [3] was used without any transadaptation as the survey tool. This being a study conducted during lockdown and pandemic, hybrid approach to collect the data was used. The questionnaire was made available to the participants via Google form, data was also collected through face-to-face interview. Participants who were unable to visit for a face-to-face interview, google form link of the questionnaire were shared with them. The language of the questionnaire was English. The informed consent form appeared at the beginning of the survey in Google form; if participants proceeded to complete the survey questionnaire that was indicative of their informed consent for participation in this study. Similarly, written and verbal consent was taken prior to the face-to-face interview mode. The informed consent was signed by the participants.
The questionnaire consisted of 20 questions, which were grouped into six sections.
Section 1: The demographic details: The socio demographic details which consists of basic questions about date of birth, gender, marital status, country, educational level, occupation, annual salary. Some details about duration of hearing loss and type and duration of amplification device used. These were close ended questions with multiple choices, where the client has to choose appropriate answer from the given choice about the type, degree and laterality of hearing loss, and type of amplification device used and duration of hearing aid usage before and after lockdown.
Section 2: This contained questions regarding extent of difficulties and concerns affecting the participants during the COVID-19-imposed lockdown period. Domains such as buying batteries for hearing device, fixing device damage and fitting hearing aids were present and the participants had to grade on 4-point Likert scale for each of the domains based on the level of problems perceived by self.
Section 3: This included questions where participants had to rate/ indicate how strongly they agree or disagree that they had found the causes interrelating with their concerns such as for example closing of hearing aid clinics or companies, support from government and lack of tele audiological services.
Section 4: Frequency of different problems experienced by the users were rated in this section, such as hearing difficulties, hearing related difficulties and communication through telephone, mobile, use of TV.
Section 5: This included different possible solutions for the challenges and the hearing aid users / participants had to indicate how strongly thy agree or disagree with the expected solutions such as increasing awareness for tele-services and train hearing care professionals for providing tele audiological services.
Each of the above-mentioned sections also included an option for mentioning any ‘additional thoughts or ideas’, where the participant can respond with descriptive sentences.
As the original questionnaire was prepared based on the participants in country such as Jordan, and were not suitable to Indian scenario, it was not made optional to skip the questions if felt not relevant by the participants. The questions related to few demographic details such as income status, state were made optional to attempt.
Audiologists from different clinical setups were contacted, explained the purpose and method of the study, with the consent from both audiologists and the hearing aid users, the participants were recruited for the study. The participants were requested to respond to the questionnaire. The detail of type, degree, configuration of hearing loss was verified from their recent audiograms. The availed data or responses from the participants were analyzed after discussion with the statistician using descriptive statistics.
Results
Section 1-Demographic Details: This study consisted of responses obtained from 31 participants with hearing loss (aged > 18 years) who used hearing amplification devices. Among them 24 participants (77.4%) were male whereas 7 participants (22.6%) were female. Sociodemographic characteristics of 31 participants which include age, marital status, educational level, profession and years of working are mentioned in Table 1.
| Variables | No. of Participants | Percentage | |
|---|---|---|---|
| Age | Less than 30 years | 3 | 9.67% |
| 30-64 years | 24 | 77.41% | |
| More than 65 years | 4 | 12.90% | |
| Single | 16.1% | ||
| Married | 20 | 64.5% | |
| Widowed | 6 | 19.4% | |
| Marital Status Educational Level | Elementary | 2 | 6.5% |
| Intermediate | 4 | 12.9% | |
| High School | 9 | 29% | |
| Diploma | 4 | 12.9% | |
| Bachelor | 6 | 19.4% | |
| Master | 4 | 12.9% | |
| PhD | 2 | 6.5% | |
| Occupation | Non- worker | 5 | 16.1% |
| Healthcare provider | 4 | 12.9% | |
| Teacher | 7 | 22.6% | |
| Engineer | 3 | 9.7% | |
| Professor | 1 | 3.2% | |
| Retired | 4 | 12.9% | |
| Others | 7 | 22.6% | |
| Years of work experience | 1-5 years | 4 | 15.4% |
| 6-10 years | 2 | 7.7% | |
| 11-15 years | 6 | 23.1% | |
| 16-20 years | 3 | 11.5% | |
| More than 20 years | 11 | 42.3% | |
Table 1: Socio-demographic characteristics of participants.
| Statement | Serious problem | Moderate problem | Minor problem | Not at all a problem |
|---|---|---|---|---|
| Buying batteries for hearing device | 7 | 18 | 4 | 2 |
| 22.58% | 58.06% | 12.90% | 6.45% | |
| Fixing device damage | 15 | 7 | 8 | 1 |
| 48.39% | 22.58% | 25.81% | 3.22% | |
| Replacing or repairing ear mold or ear mold tubing | 10 | 15 | 5 | 1 |
| 32.26% | 48.39% | 16.13% | 3.22% | |
| Fitting hearing aids | 9 | 13 | 8 | 1 |
| 29.03% | 41.94% | 25.81% | 3.22% | |
| Continuing language and speech therapy | 5 | 7 | 8 | 11 |
| 16.13% | 22.58% | 25.81% | 35.48% | |
| Distance education or/ and work | 6 | 7 | 14 | 4 |
| 19.35% | 22.58% | 45.16% | 12.90% |
Table 2: The hearing concerns of participants during COVID-19 outbreak.
Regarding the nature of hearing loss and the use of hearing aids, moderately severe was prevalent severity seen in right ear among all participants where as severe hearing loss was prevalent severity seen in left ear among all participants, (Figure 1) where as both the right and left ear, sensorineural hearing loss was the most common (Figure 2).
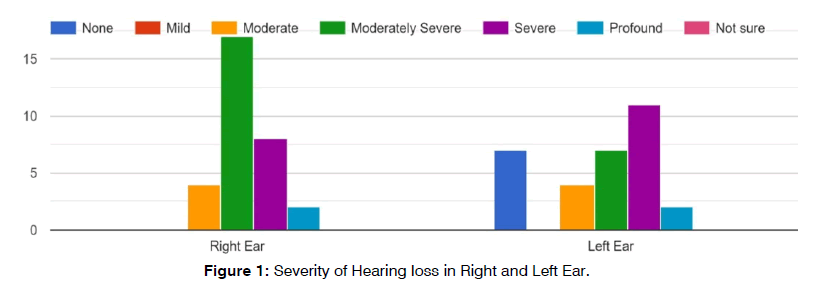
Figure 1: Severity of Hearing loss in Right and Left Ear.
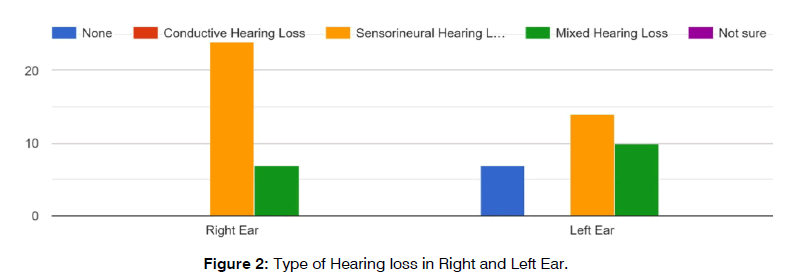
Figure 2: Type of Hearing loss in Right and Left Ear.
With regard to hearing aids, behind the ear hearing aids were widely used which was followed by receiver in the canal hearing aids and completely in canal hearing aids.
The Hearing Concerns and Problems in Participants during COVID-19 Outbreak: Regarding the hearing concerns and problems experienced by them during COVID-19 outbreak, purchasing batteries and repairing the hearing aids during pandemic was one of the most commonly reported problem by the participants. Few other concerns included, problem in repairing or replacing the ear mold or ear mold’s tubing, programming of hearing devices.
Reasons for Anticipating COVID-19 to be a Challenging Situation for Individuals with Hearing- Impaired: Majority of the participants were agreed for all the statements in this section. The common challenges faced by individuals with hearing impairment during COVID 19 are the non-functioning hearing centres, the curfew which was enforced and the health regulations by Ministry of health. According the participants, usage of tele-audiology services were inhibited due to poor service quality and unenthusiastically professional-patient communication, which needs to be improved also the teleaudiology and speech services were unavailable at most hearing or speech centers. The vast majority of speech language pathologists and audiologists were untrained in tele-audiology and speech services. Another factor that could have hindered the tele audiology services is social concentration on non-hearing issues more and also, there was lack of transportation during pandemic. Table 3 shows the response of participants of all 9 questions in this section.
| Statement | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| Most of hearing companies and speech centers had been closed | 3 | 26 | 1 | 1 | - |
| 9.68% | 83.86% | 3.23% | 3.23% | - | |
| Ministry of Health provided no hearing services during strict curfew | 3 | 17 | 6 | 5 | - |
| 9.68% | 54.84% | 19.35% | 16.13% | - | |
| Most hearing companies and speech centers offered no tele-audiology and speech services | 11 | 13 | 5 | 1 | 1 |
| 35.48% | 41.93% | 16.13% | 3.23% | 3.23% | |
| Most audiologists and speech language pathologists are not trained in tele-audiology and speech services | 9 | 13 | 7 | 2 | - |
| 29.03% | 41.93% | 22.58% | 6.45% | - | |
| Individual with hearing impairment unfamiliar with use of tele- audiology services | 12 | 14 | 5 | - | - |
| 38.71% | 45.16% | 16.13% | - | - | |
| Unfavorable attitude or circumstances prevented use of tele-audiology services such as poor quality of services and unenthusiastically professional-patient communication. | 7 | 17 | 7 | - | - |
| 22.58% | 54.84% | 22.58% | - | - | |
| Cost of services (e.g., hearing aid batteries) and expensive home delivery charges | 7 | 18 | 4 | 2 | - |
| 22.58% | 58.06% | 12.90% | 6.45% | - | |
| Society had focused on other non- hearing matters during the COVID-19-imposed lockdown | 9 | 15 | 5 | 2 | - |
| 29.03% | 48.39% | 16.13% | 6.45% | - | |
| Lack of transport during the COVID-19-imposed lockdown | 11 | 15 | 4 | 1 | - |
| 35.48% | 48.39% | 12.90% | 3.23% | - |
Table 3: The reasons reported by 31 participants that caused their struggles during pandemic.
The Negative Impact of the COVID-19-Imposed Lockdown on Hearing Technology Users: Participants mentioned that they faced difficulties with hearing which limited their personal or social life very frequently Along with hearing difficulties, hearing related complications such as ear infections, ear ringing and vertigo were also commonly reported. Communication difficulties with clients, co-workers or family members through phone calls, social media and video calls were another aspect that impacted their quality of life during the pandemic. Hearing loss has enabled to feel more anxious and depressed than normal, Speech and language skills had begun to deteriorate also academic or professional performance had deteriorated as reported frequently by most of the participants. Table 4 summarized the response of participants on impact on the user of hearing technology devices due to COVID-19 lockdown.
| Statement | Very Frequently | Somewhat Frequently | Not too Frequently |
|---|---|---|---|
| Hearing difficulties | 6 | 22 | 3 |
| 19.35% | 70.97% | 9.68% | |
| Hearing-related problems such as ear ringing, ear infections, vertigo | 7 | 14 | 10 |
| 22.58% | 45.16% | 32.26% | |
| Communication problems with family members, co-workers, or clients through face- face, video calls, phone calls, and social media | 9 | 20 | 2 |
| 29.03% | 64.52% | 6.45% | |
| Greater than normal embarrassment when socializing | 8 | 19 | 4 |
| 25.81% | 61.29% | 12.90% | |
| Arguing more than usual with people around you | 8 | 14 | 9 |
| 25.81% | 45.16% | 29.03% | |
| Difficulties when listening to media such as TV, radio, record | 12 | 17 | 2 |
| 38.71% | 54.84% | 6.45% | |
| Difficulties with hearing that limit your personal or social life | 15 | 9 | 7 |
| 48.39% | 29.03% | 22.58% | |
| Feeling more depressed and anxious than usual because of hearing loss | 9 | 16 | 6 |
| 29.03% | 51.61% | 19.35% | |
| Deteriorations had been noticed in speech and language skills | 8 | 16 | 7 |
| 25.81% | 51.61% | 22.58% | |
| Deterioration had been noticed in academic or work performance | 11 | 17 | 3 |
Table 4: The impact of the COVID-19 lockdown on 31 participants.
Solutions to Minimize the Effects of Hearing during Pandemic: The solutions proposed here was to reduce the impact faced by hearing aid users and the agreements on these solutions were evaluated eliciting participant’s response. Table 5 shows that participants agreed for each of eight solutions were helpful in dealing with the pandemic. Participants agreed on a set of proposed solutions which are described further. Through tele-audiology and speech therapy, speech and hearing services can be provided by specialists. Speech language pathologist and Audiologists can be trained to practice tele- audiology and speech services. Individual with hearing impairment can be encouraged to use tele- audiology services, Awareness about the importance of tele-audiology services needs to be increased among individuals and other common difficulties like availing hearing aid batteries and technical supports can be delivered free or at a reasonable cost by hearing aid companies
| Statement | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| Offering hearing services by hearing specialized sites through tele-audiology practice | 6 | 24 | 1 | - | - |
| 19.35% | 77.42% | 3.23% | - | - | |
| Offering hearing services by Ministry of Health during the COVID-19 outbreak | 11 | 16 | 3 | 1 | - |
| 35.48% | 51.61% | 9.68% | 3.23% | - | |
| Providing online speech and language therapy sessions to those in need | 6 | 13 | 3 | 8 | 1 |
| 19.35% | 41.93% | 9.68% | 25.81% | 3.23% | |
| Training audiologist and speech language pathologist to use tele- audiology and speech services | 8 | 17 | 5 | 1 | - |
| 25.81% | 54.83% | 16.13% | 3.23% | - | |
| Training individual with hearing impairment to use tele- audiology services | 11 | 15 | 5 | - | - |
| 35.48% | 48.38% | 16.13% | - | - | |
| Increasing awareness about the importance of tele-audiology services among healthcare providers and patients | 10 | 17 | 2 | 2 | - |
| 32.26% | 54.84% | 6.45% | 6.45% | - | |
| Monitoring the prices of hearing services offered by hearing companies | 12 | 12 | 3 | 2 | 2 |
| 38.71% | 38.71% | 9.68% | 6.45% | 6.45% | |
| Delivery of hearing aid batteries by hearing companies free or at reasonable charges | 10 | 16 | 3 | 2 | - |
Table 5: Proposed solutions addressed by 31 participants to reduce the impacts of hearing problems related to pandemic.
Discussion
The aim of the study was to investigate and address the concerns of hearing aid users as a result of the COVID- 19-imposed lockdown in India. A total of 31 individuals contributed in the study, different aspects related to COVID-19 pandemic were focused such as challenges during this time period and causes for the issues. The study also aimed to elicit potential strategies for solving or at least limiting the detrimental impact of these challenges in a practical manner. A study discussed that hearing loss affects the quality of life and impacts on psychological conditions also reported possibilities of depression, anxiety, and social isolation. Among hearing aid users during COVID-19 pandemic [16-23]. Their study outcome mainly focused on impact of mask, social distancing as a communication barrier for the hearing aid users and possible solutions such as use of transparent mask, some compensatory strategy [24]. The importance of tele rehabilitation was also discussed in their study which was already focused in our study outcome and outcome suggested need of increasing awareness and train hearing care professionals for increasing the implementation of tele services. Most of the users chosen tele services as a better solution during COVID-19 pandemic. Another study showed effect of COVID-19 on Cochlear Implant Users, during the COVID-19 outbreak, where the majority of respondents reported a range of issues with the use, management, and maintenance of Cochlear Implants [13]. During lockdown, the majority of responders said their children were unable to attend AVT. The responders expressed concerns about the device’s care and maintenance. The headpiece, battery compartment, speech processor, microphone, cables, battery, and battery charger are reported to be the most common repair difficulties with cochlear implants in children. However, professionals of CI programs must provide proper, consistent, and ongoing guidance on the maintenance of these components in order to prevent technical failures of devices in a more scientific manner during pandemic situations. Due to the lockdowns with limited services some patients couldn’t attend followups for their device programming, which subsequently affected their child’s performance [16]. With support to the current study the limited technical services during the lockdown period also chosen as an important problem for hearing aid users which already discussed as an outcome our study. The outcomes of the study done by Saxena13 also mentioned the importance on tele rehabilitation and its effectiveness which also supports the outcomes of the current study.
Outcomes of the study done by Alqudah S3 also reported that certain needs such as buying batteries for hearing aid, fixing damaged device, ear mold Replacement or repairing or earmold tubing Fitting hearing aids. are considered as a serious to moderate problem, which supports findings of the current study, also maximum of the respondents agreed with specific causes for the challenging situations such as, lack of hearing services Ministry of Health during strict curfew, lack of tele-audiology and speech services, inadequate training of professionals in tele-audiology and speech services, unfamiliarity of the users with use of tele-audiology services. The outcomes of the current study also show similar findings with respect to the causes for challenging situation during COVID-19 curfew. Similarly supporting to the current study outcome, Alqudah [3] explored that, hearing aid users reported higher frequency of occurrence for list a list of issues such as, hearing difficulties ,communication problems with family members, coworkers, or clients through faceface, video calls, phone calls, and social media, Greater than normal embarrassment when socializing , Feeling more depressed and anxious than usual because of hearing loss, Difficulties when listening to media such as TV, radio, record,during the lockdown period. Findings from the study done by Alqudah [3] as well as current study reported that, Hearing aid users agreed with a list of possible solutions to overcome various challenges during the COVID-19 pandemic such as, offering hearing services by hearing specialized sites through tele audiology practice, offering hearing services by Ministry of Health during the COVID-19 outbreak, providing online speech and language therapy sessions to those in need, Training audiologist and speech language pathologist to use teleaudiology and speech services. Training Individual with hearing impairment to use tele audiology service increasing awareness about the importance of tele-audiology services among healthcare providers and patient.
Conclusion
In conclusion, this study reported the main obstacles described by hearing aid users during the COVID-19 outbreak to aid in the development of management options using tele mode of rehabilitation. Main concern by the hearing aid users were lack of services and availability of accessories, batteries and ear mold. Whereas importance was given tele mode of service was given the most priority as a possible solution. So, preferences for increasing awareness among hearing aid users and training professionals for providing tele service is an important aspect which was maximally chosen by the users. While discussing some limitations of the study, a list of modifications also needed in the study tool because it is originally designed for Jordan population, so some specific modification based on Indian scenario is also needed such as, changing the currency option in the annual income from Jordan dollar to INR, some recent problems such as communication difficulties due to use of mask, face shield, and social distancing, can be added in the questionnaire. The current study is a pilot study so the sample size is less in number which can be increased for more generalized outcome. In future directions we can extend the study with more sample size, and a modified version of the questionnaire can be used with added the limitation of the current study tool.
References
- A guide to WHO’s guidance on COVID-19. 2020.
- Tavanai E, Rouhbakhsh N, Roghani Z. A review of the challenges facing people with hearing loss during the COVID-19 outbreak: toward the understanding the helpful solutions. Aud Vestib Res. 2021;30(2):62-73.
- Alqudah S, Zaitoun M, Alqudah O, Alqudah S, Alqudah Z. Challenges facing users of hearing aids during the COVID-19 pandemic. Int J Audiol. 2021;60(10):747-53.
- Boldrini T, Schiano Lomoriello A, Del Corno F, Lingiardi V, Salcuni S. Psychotherapy during COVID-19: How the clinical practice of Italian psychotherapists changed during the pandemic. Front Psychol. 2020;11:591170.
- Umashankar A, Prabhu P. Effect of Covid-19 on individuals with hearing impairment in India. J Clin Diagn Res. 2020;14(8):10-7860.
- Fortnum HM, Davis A, Summerfield AQ, Marshall DH, Davis AC, Bamford JM, et al. Prevalence of permanent childhood hearing impairment in the United Kingdom and implications for universal neonatal hearing screening: questionnaire based ascertainment study Commentary: Universal newborn hearing screening: implications for coordinating and developing services for deaf and hearing impaired children. BMJ. 2001;323(7312):536.
- Swanepoel DW, Hall JW. Making audiology work during COVID-19 and beyond. Hear J. 2020;73(6):20-2.
- Edwards M, Stredler-Brown A, Houston KT. Expanding Use of Telepractice in Speech-Language Pathology and Audiology. Volta Rev. 2012;112(3).
- Swanepoel DW, Clark JL, Koekemoer D, Hall Iii JW, Krumm M, Ferrari DV, et al. Telehealth in audiology: The need and potential to reach underserved communities. Int J Audiol. 2010;49(3):195-202.
- Swanepoel DW, Hall III JW. A systematic review of telehealth applications in audiology. Telemed J E Health. 2010;16(2):181-200.
- Bush ML, Thompson R, Irungu C, Ayugi J. The role of telemedicine in auditory rehabilitation: A systematic review. Otol Neurotol. 2016;37(10):1466.
- Tao KF, Brennan-Jones CG, Capobianco-Fava DM, Jayakody DM, Friedland PL, Swanepoel DW, et al. Teleaudiology services for rehabilitation with hearing aids in adults: A systematic review. J Speech Lang Hear Res. 2018;61(7):1831-49.
- Saxena U, Chacko G, Kumar SB, Nagabathula V, Damarla V, Saxena U, et al. Effect of COVID-19 on cochlear implant users: parental perspectives. Clin Arch Commun Disord. 2021;6(1):12-7.
- Luey HS, Glass L, Elliott H. Hard-of-hearing or deaf: Issues of ears, language, culture, and identity. Social Work. 1995;40(2):177-82.
- Taylor B. Changes in hearing aid benefit over time: An evidence-based review. Audiol Online. 2007.
- Pereira AM, Melo TM. Repair issues associated with cochlear implants external components: The influence of age and time of use. Revista CEFAC. 2014;16:1419-25.
- Bakhit M, Rohbakhsh N, Delphi M. Evaluating hearing disability using Persian version of quantified Denver scale of communication function in adults with slight to profound hearing loss. J Res Rehabili Sci. 2012;8(5):818-26.
- Campos PD, Ferrari DV. Teleaudiology: evaluation of teleconsultation efficacy for hearing aid fitting. J Soc Bras Fonoaudiol. 2012;24:301-8.
- Chang HP, Ho CY, Chou P. The factors associated with a self-perceived hearing handicap in elderly people with hearing impairment—results from a community-based study. Ear Hear. 2009;30(5):576-83.
- Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging. 2012:159-63.
- Eikelboom RH, Atlas MD. Attitude to telemedicine, and willingness to use it, in audiology patients. J Telemed Telecare. 2005;11(2_suppl):22-5.
- Eikelboom RH, Swanepoel DW. International survey of audiologists' attitudes toward telehealth. Am J Audiol. 2016;25(3S):295-8.
- Shukla A, Harper M, Pedersen E, Goman A, Suen JJ, Price C, et al. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck Surg. 2020;162(5):622-33.
- Ten Hulzen RD, Fabry DA. Impact of hearing loss and universal face masking in the COVID-19 era. InMayo Clinic Proceedings. 2020;95(10):2069-2072.
1TMC Fellow in Speech and Swallow Therapy, Department of Head and Neck Oncology, Tata memorial Hospital, Mumbai, India
2Grade 1 -Clinical Supervisor (SLP), Sri Aurobindo Institute of Medical sciences, Indore, India
3Associate Professor, BSHRF, Dr. S.R. Chandrasekhar Institute of Speech and Hearing, Lingarajapuram, Bangalore, India
Send correspondence to:
A. Srividya
Associate Professor, BSHRF, Dr. S.R. Chandrasekhar Institute of Speech and Hearing, Lingarajapuram, Bangalore, India, Email: the.srividya@gmail.com
Tel: 9880938138
Paper submitted on July 27, 2023; and Accepted on August 25, 2023
Citation: Ghadei A, Kumar A, Thontadarya S, Srividya A. Challenges Faced by Individuals with Hearing Impairment during COVID-19 Pandemic Lockdown – A Pilot Study. Int Tinnitus J. 2023;27(2):126-134.


