The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 28, Issue 1 / June 2024
Research Article Pages:157-162
10.5935/0946-5448.20240023
Effect of Septoplasty On relieving contact point headache
Authors: Lana Shahabaddin*, Abdulkhaliq Emin, Hanna Kasho
PDF
Abstract
Introduction: The idea that headaches can be triggered by nasal or sinus abnormalities is well-established. The proposed mechanism involves mucosal contact between the nasal septum and the middle turbinate, which acts as a mechanical stimulus, triggering an axonal reflex that result in pain. Aim of the Study: This study aims to evaluate the pain relief in patients with septal deviation and contact point headaches over a 6-month postoperative septoplasty follow-up period. Patients and Methods: Fifty patients with nasal septal deviation and headaches who underwent septoplasty surgery at Rizgary Teaching Hospital in Erbil between January 15, 2022, and January 15, 2023, were included in the study. The patients' ages ranged from 18 to 38 years, with an equal distribution of males (50%) and females (50%). Patients whose pain and headaches were relieved by the application of a piece of cotton soaked in 10% lidocaine to the contact point were included. Pain complaints were assessed using a Visual Analog Scale (VAS) both preoperatively and 6 months postoperatively. The NOSE scale was also used preoperatively and at the 6-month postoperative mark to evaluate the outcome of the septoplasty. Final data were analyzed using SPSS and descriptive statistics, with pain severity categorized as 0-3 mild, 4-6 moderate, and 7-10 severe. Results: Most patients reported a decrease in pain intensity postoperatively, with 33 patients (66%) experiencing complete relief. The difference between preoperative and postoperative VAS pain scores was statistically significant (p = 0.001). Conclusion: Removing contact points in patients with contact point headaches are highly effective in carefully selected patients.
Keywords: Septoplasty, Contact point, Headache, Sluder neuralgia.
Introduction
Reaching the correct diagnosis in patients with facial pain is challenging because many patients come with fixed ideas about the cause of their pain [1]. Headache disorders are revealed as one of the major public-health concerns globally and in all countries and world regions [2].
In the general population, more than 50% of the adults indicate that they have suffered from headache and almost 5% (9% of women) suffer from chronicdaily headache [3].
For centuries, conceptual understanding of headache causation has been attributed to anatomic abnormalities of the nose and paranasal sinuses [4]. In 1920, Sluder described neuralgia of the sphenopalatine ganglion as a possible cause of chronic headaches. In the 1940s, Wolf described the study of referred nasal pain after application of stimuli to internal structures of the nose [5]. However, interest in so-called rhinogenic headaches increased with the advent of the endoscope; further spurring advancements for more precise endonasal surgical techniques in recent decades [6]. RCPH Rhinological contact point headache is distinguished by several possible anatomical abnormalities such as septal spurs or middle turbinate disorders such as hypertrophic, deformed or hyperpneumatized (concha bullosa), in the absence of inflammation of nasal mucosa. The diagnosis of RCPH needs a multidisciplinary approach, which is often misdiagnosed. Patients with headache in the absence of inflammation of the sinonasal area should be examined by a neurologist, ophthalmologist, dentist, and internist to rule out other causes. RCHP is quickly detectable and quantified by sinonasal endoscopy or computed tomography [7-11]. A common diagnostic method used to identify possible surgical candidates is the application of local anesthetics and decongestants at the contact point relieves the headache which confirms the diagnosis of the RCPH [12]. The proposed mechanism in such cases is the mucosal contact between the nasal septum and the middle turbinate acting as a sensory stimulus to produce an axonal reflex resulting in the reported pain hich creates a sensory stimulus resulting in release of substance P and stimulation of unmyelinated C fibers that is responsible for the headache [13,14]. RCPH is an important etiology for secondary headache which can be treated by surgical or medical therapy. Topical nasal decongestant or steroids can relieve the RCPH, however, the long-term relieve needs surgical interventions, endoscopic surgery is an ideal technique to relieve mucosal contact point headache [15].
Aim of the Study
This study aimed to diagnose contact point headaches in patients with nasal septal deviation and evaluate headache relief following septoplasty.
Materials and Methods
The study was conducted at Rizgary Teaching Hospital in Erbil from January 15, 2022, to January 15, 2023. We performed a prospective analysis of 50 patients (25 male and 25 female), aged between 18 and 38 years. These patients presented with nasal obstruction and contact point headaches of rhinogenic origin, particularly frontal, temporal, parietal, or periorbital pain, persisting for over a year. All patients had a long-standing history of mild to moderate headaches and had not experienced satisfactory relief from previous treatments. Preoperative evaluations included a detailed medical history, complete ENT examination, diagnostic nasal endoscopy, and assessment of allergy status. Patients with signs of inflammatory diseases such as nasal polyps, mucopurulent discharge, or hyperplastic mucosa were excluded. Additionally, all patients underwent consultations with Neurologists, Ophthalmologists, and Dentists. Preoperative headache intensity was assessed using a 10-point Visual Analog Scale (VAS), where 0 indicated no headache and 10 represented the most severe pain.
Patients were questioned about their use of analgesics or other medications and their effectiveness in relieving their symptoms. After applying a topical decongestant, xylometazoline 0.1%, to the nasal passages, a small piece of cotton soaked in 10% lidocaine was applied to the contact points using an endoscope. Patients with clear contact points identified by endoscopy, whose headaches responded to this application, were included in the study. The baseline NOSE score was recorded a week before surgery, and all patients underwent septoplasty under general anesthesia. Follow-ups were conducted for six months postoperatively.
Inclusion Criteria:
• Patients with recurrent contact point headaches for more than one year.
• Presence of contact between the inferior turbinate and septum, middle turbinate and septum, or other contact areas on clinical and endoscopic examination.
• Positive local anesthesia test.
Exclusion Criteria:
• Signs of inflammatory disease, such as nasal polyps, mucopurulent discharge, or hyperplastic mucosa.
• Patients with a history or diagnosis of non-sinus headache causes, including migraines, vascular disorders, neuralgias, cervical spine disorders, temporomandibular joint disorders, or ophthalmic refractive issues. These patients were referred for Neurological, Ophthalmological, and Dental consultations.
Data Collection
The following information was collected: age, gender, headache onset, course, duration, pain location, radiation areas, pain characteristics (dull, aching, pulsating, or sharp), and pain severity. Nasal decongestion was achieved with xylometazoline 0.1% spray for better examination. Rhinoscopy focused on septal deviations, spurs, middle turbinate hypertrophy, uncinate process size and abnormalities, and bulla ethmoidalis size.
During headache attacks, a local anesthetic test was performed. A piece of cotton soaked in 10% lidocaine (xylocaine) was placed in the nose at the site of contact between the middle turbinate and septum, between the septum and inferior turbinate, or other suspected contact areas on the ipsilateral side of the headache, and then on the contralateral side. The cotton was left for 3-5 minutes until the local anesthetic became effective. Patients were asked if their headache severity decreased, and the degree of decrease was noted as a percentage of the original headache. A positive test was defined as a reduction in headache severity by more than 50%. The nose was reexamined by anterior rhinoscopy and endoscopy and reporting any abnormalities in septum and middle turbinate. The test was repeated at least twice on different occasions for each patient.
Results
Fifty patients who had nasal obstruction and headache especially frontal, temporal, parietal, or periorbital pain particularly at the medial canthus were included in the study.
Out of the 50 patients, 25 were male (50%) and 25 were female (50%). Patients age were 18-38 years with an average age of (26+6) years. Age distribution (Table 1).
| Age(years) | Frequency | Percentages |
|---|---|---|
| <20 | 6 | 12 |
| 20-24 | 17 | 34 |
| 25-29 | 14 | 28 |
| 30-34 | 7 | 14 |
| 35+ | 6 | 12 |
| total | 50 | 100 |
Table 1: Distribution of sample by age
Nasal obstruction and headache was the most common compliant 100%, followed by facial pain 78%, postnasal discharge 46%, hyposmia 32 and the least was epistaxis 12% (Table 2).
| Incidence of symptoms | Frequency | % |
|---|---|---|
| Nasal obstruction | 50 | 100 |
| Facial pain | 39 | 78 |
| Headache | 50 | 100 |
| hyposmia | 16 | 32 |
| epistaxis | 6 | 12 |
| Postnasal discharge | 23 | 46 |
Table 2: Distribution of sample by incidence of symptoms
Out of the 50 patients who had distinct contact points in endoscopy and whose headache had responded to local anesthesia, Headaches were bilateral in 34 patients (68%) and unilateral in 16 (32%). Region of pain was as follows (Table 3).
| Region | Frequency | % |
|---|---|---|
| Frontal region | 19 | 38 |
| Temporal region | 11 | 22 |
| Periorbital region | 14 | 28 |
| Parietal region | 6 | 12 |
| Total | 50 | 100 |
Table 3: Distribution of sample by region of pain
Thirty four of 39 patients with facial pain reported a completed cure of pain and 5 patients reported no changes in their complaints. This result statistically was significant p<0.001, 8 of 16 patients with hyposmia reported improvement (p<0.063), 6 of 6 patients with epistaxis reported cure and 16 of 23 patients with postnasal discharge reported improvement in their complaints (p=0.002) as shown in (Table 4).
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| No. of patients improved | No. of patients not improved | |||
| Symptoms | Frequency | P value | ||
| Nasal obstruction | 50 | 47 | 3 | <0.001** |
| -100% | -94% | -6% | ||
| Facial pain | 39 | 34 | 5 | <0.001* |
| -78% | -87.10% | -12.90% | ||
| Headache | 50 | 44 | 6 | 0.015** |
| -100% | -87.50% | -12.50% | ||
| Hyposmia | 16 | 8 | 8 | <0.063* |
| -32% | -50% | -50% | ||
| Epistaxis | 6 | 6 | 0 | NA |
| -12% | -100% | 0% | ||
| Postnasal discharge | 23 | 16 | 7 | 0.002* |
| -46% | -69.50% | -30.50% | ||
**Fisher's Exact Test was used
Table 4: Post-operative symptoms results
Out of 50 patients 47 patients noted relief of nasal obstruction which was statistically highly significant (p<0.001). Regarding Nose scale pre and postoperative outcome summarized (Table 5).
| Nose Score Components | Preoperative Mean±SD | Postoperative Mean±SD | p value |
|---|---|---|---|
| Nasal congestion | 1.99±0.5 | 0.62±0.42 | <0.001 |
| Nasal blockage | 2.00 ±0.7 | 0.51±0.51 | |
| Trouble breathing through nose | 2.01±0.99 | 0.03 ±0.30 | |
| Trouble sleeping | 1.63±1.12 | 0.09±0.35 | |
| Unable to get enough air through nose during exercise | 1.85±1.00 | 0.12±0.32 | |
| Total score (out of 100) | 47.32±22.42 | 8.32±8.21 |
Table 5: Nose Scale Results
Out of 50 patients 44 patients reported a postoperative absence of headache or a decrease in the intensity. The overall success rate for improvement of patient’s headache in our study was approximately 87.5%. 65.6% patients reported complete relief of pain following surgery and (21.9%) reported improvement “reduced headache” which they no longer considered significant. 12.5% reported no changes in headache post-operatively. None of the patients reported an increase in the frequency or intensity of their headaches postoperatively.
Comparing preoperative and 6-month postoperative headache, Results showed significant decrease in the Ranks of headache scores (p<0.001), by Wilcoxon sign rank test.
Patient’s headache responses to surgical corrective treatment(s) were statistically significant (P < .001) as shown in (Figure 1). Complete cure occurred in 65.6%.
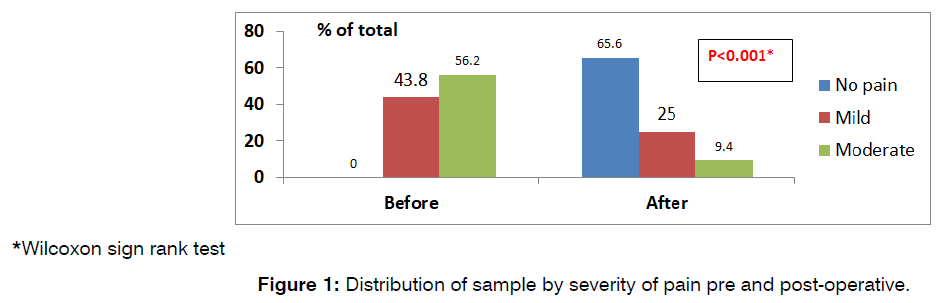
*Wilcoxon sign rank test
Figure 1: Distribution of sample by severity of pain pre and post-operative.
Discussion
Rhinologic contact point headache remains a controversial issue. While contemporary medicine acknowledges contact point headache as a cause of headache, the specific role of rhinologic contact point headache continues to be debated in the literature. Numerous studies on patients with nasal anatomical abnormalities, such as nasal septal deviation, who have undergone septoplasty, indicate that heaaches are a common preoperative complaint. Given that these headaches often respond well to surgical treatment, postoperative follow-ups can clarify the relationship between headache symptoms and nasal anatomical abnormalities, as well as the impact of surgery on headache recovery rates in such patients.
In our study, the average age of the patients was 26 years, ranging from 18 to 38 years. This is similar to another study involving 40 patients scheduled for septoplasty, where the mean age was 31.5 years (ranging from 18 to 55 years).
Regarding preoperative symptoms, all 50 patients (100%) had nasal obstruction and headaches. Additionally, 25 patients (78.1%) experienced facial pain, 15 patients (46.8%) had postnasal drip, 10 patients (31.2%) suffered from hyposmia, and 4 patients (12.5%) had epistaxis [16]. This aligns closely with a study by Hakmi et al., where among 209 patients who underwent surgery for a deviated nasal septum, 95.4% had nasal obstruction, 12% had nasal discharge, 7.3% experienced loss of smell, 6.4% had facial pain, 12.7% had headaches, 3.6% had postnasal drip, 8.2% snored, and 3.6% had epistaxis. The symptom percentages were similar to our study, except for headaches, as our study focused on contact headaches as the major parameter [17].
In a study by 72.4% of participants suffered from nasal congestion, 63.2% from oral breathing, 46% from headaches, and 17.3% from epistaxis [18]. These findings correspond to those reported by Low and Willatt in their pre-septoplasty study on 75 patients, where 57.3% experienced oral breathing, 48% had headaches, and 21.3% had epistaxis [19].
In terms of headache locations, our study found that 12 patients (37.5%) reported frontal headaches, 9 (28.12%) had periorbital headaches, 7 (21.8%) experienced temporal headaches, and 4 (12.5%) had parietal headaches. In comparison, the study by Ghazipour reported that 31 patients (68.8%) had frontal headaches, 20 (44.4%) had periorbital headaches, 17 (37.7%) had temporal headaches, and 14 (31.1%) had facial headaches.
Six months post-surgery, our study revealed a significant difference in headache intensity compared to pre-operative levels, with a p-value of <0.001. Specifically, 21 patients (65.6%) reported full recovery, and 7 patients (21.8%) noted a decline in pain intensity.
Conducted nasal surgery for contact point headaches and reported improvement in 91% of patients post-surgery. Complete relief and significant improvement were observed in 43% and 47% of patients, respectively [20-23]. After corrective surgery, Altin et al. demonstrated a 96% improvement in Contact Point Headaches (CPH), while Bilal et al. reported a 92% improvement in headache levels [24].
Our study also showed a significant improvement in NOSE scores six months postoperatively, consistent with two other studies that reported significant improvement in all NOSE score symptoms post-septoplasty. Additionally, there was a statistically significant improvement in headache intensity post-operation using the VAS, which aligns with several other studies [25].
Conclusion
Our findings suggest that surgical removal of contact points can alleviate headaches when a demonstrated contact point headache responds to local anesthetics. Due to potential relapse in some long-term studies, we recommend 10-20-year follow-ups to assess the long-term effectiveness of the surgery and the rate of relapse.
Limitation
A limitation of our study is the short-term follow-up period of six months.
References
- Faris C. Scott-Brown’s Otorhinolaryngology, Head and Neck Surgery, 7th edn. Ann R Coll Surg Engl. 2018.
- Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954-76.
- Bugten V, Fossum M, Nilsen AH. Sinus or nasal surgery alleviates headache symptoms: A prospective study. AOR. 2018.
- Altin F, Haci C, Alimoglu Y, Yilmaz S. Is septoplasty effective rhinogenic headache in patients with isolated contact point between inferior turbinate and septal spur?. Am J Otolaryngol. 2019;40(3):364-7.
- Patel ZM, Setzen M, Poetker DM, DelGaudio JM. Evaluation and management of “sinus headache” in the otolaryngology practice. Otolaryngol Clin North Am. 2014;47(2):269-87.
- Graff-Radford SB, Abbott JJ. Temporomandibular disorders and headache. Oral Maxillofac Surg Clin North Am. 2016;28(3):335-49.
- Pasha R, Soleja RQ, Ijaz MN. Imaging for headache: what the otolaryngologist looks for. Otolaryngol Clin North Am. 2013;47(2):187-95.
- Yi HS, Kwak CY, Kim HI, Kim HY, Han DS. Rhinogenic headache: standardization of terminologies used for headaches arising from problems in the nose and nasal cavity. J Craniofac Surg. 2018;29(8):2206-10.
- Sollini G, Mazzola F, Iandelli A, Carobbio A, Barbieri A, Mora R, et al. Sino-nasal anatomical variations in rhinogenic headache pathogenesis. J Craniofac Surg. 2019;30(5):1503-5.
- La Mantia I, Grillo C, Andaloro C. Rhinogenic contact point headache: surgical treatment versus medical treatment. J Craniofac Surg. 2018;29(3):e228-30.
- Cocuzza S, Maniaci A, Di Luca M, La Mantia I, Grillo C, Spinato G, et al. Long-term results of nasal surgery: comparison of mini-invasive turbinoplasty. J Biol Regul Homeost Agents. 2020;34(3):1203-8.
- Swain SK. Rhinogenic contact point headache–A review. Matrix Sci Medica. 2022;6(3):65-9.
- Stammberger H, Wolf G. Headaches and sinus disease: the endoscopic approach. Ann Otol Rhinol Laryngol. 1988;97(5):3-23.
- Welge?Luessen A, Hauser R, Schmid N, Kappos L, Probst R. Endonasal surgery for contact point headaches: a 10?year longitudinal study. Laryngoscope. 2003;113(12):2151-6..
- Peric A, Rasic D, Grgurevic U. Surgical treatment of rhinogenic contact point headache: an experience from a tertiary care hospital. Arch Otolaryngol. 2016;20:166-71.
- Valsamidis K, Titelis K, Rachovitsas D, Konstantinidis I, Markou K, Triaridis S. Long-term evaluation of nasal septoplasty followed by inferior turbinate cauterization for the treatment of nasal obstruction using objective and subjective methods. Arch Otolaryngol. 2018;22:284-90.
- Hakami KT, Almalki ZA, Alnemari FS, Alotaibi RM, Bajunaid FR, Hakami K, et al. A Comparison of Symptom Improvement and Outcomes After Septoplasty Alone Versus Septoplasty With Turbinoplasty. Cureus. 2023;15(3).
- Ghazipour A, Abshirini H, Pursalehan S. Sinonasal headaches and post-operative outcomes after septoplasty in patients with nasal septal deviation. Iran J Otorhinolaryngol. 2011;23(65):133-9.
- Low WK, Willatt DJ. Submucous resection for deviated nasal septum: a critical appraisal. Singapore Med J. 1992;33(6):617-9.
- Tosun F, Gerek M, Özkaptan Y. Nasal surgery for contact point headaches. J Headache Pain. 2000;40(3):237-40.
- Bilal N, Selcuk A, Karakus MF, Ikinciogullari A, Ensari S, Dere H. Impact of corrective rhinologic surgery on rhinogenic headache. J Craniofac Surg. 2013;24(5):1688-91.
- Philip P, Pratap D, Rajeshwary A, Bhat V. Subjective assessment of outcomes of septoplasty. Int J Otorhinolaryngol Clin. 2017;9(2):42-6.
- Goyal L, Swami H, Dutta A, Sahu PK, Bothra J. Correlation between subjective and objective outcomes of septoplasty in septal deviation. Int J Otorhinolaryngol Head Neck Surg. 2022;8(7):587-94.
- Folic MM, Barac AM, Ugrinovic AB, Jotic AD, Trivic AS, Milovanovic JP, et al. Effectiveness of the Treatment of Rhinogenic Headache Caused by Intranasal Contact. Ear Nose Throat J. 2023;102(9):605-10.
- Feroz S, Dawood MH, Sohail S, Daniyal M, Zafar A, Shahid UB, et al. A longitudinal prospective study of septoplasty impact on headache and allergic rhinitis in patients with septal deviation. Int J Med Res. 2023;51(11):03000605231215168.
Department of otolaryngology, Hawler medical university, Rizgari teaching hospital, Iraq
Send correspondence to:
Lana Shahabaddin
Department of otolaryngology, Hawler medical university, Rizgari teaching hospital, Iraq, E-mail: lana.a.sh.d@gmail.com
Paper submitted on June 17, 2024; and Accepted on June 19, 2024
Citation: Lana Shahabaddin. Effect of Septoplasty on Relieving Contact Point Headache. Int Tinnitus J. 2024;28(1):157-162


