The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 28, Issue 1 / June 2024
Research Article Pages:82-97
10.5935/0946-5448.20240015
High-Risk Pregnancy and Resilience: Unraveling the Links to Prenatal Anxiety and Depression
Authors: Amal I Khalil*, Howaida S Saati , Tahany E Amr
PDF
Abstract
Objective: The current study aimed to investigate the relationship between resiliency and the prevalence and severity of prenatal anxiety and depression in the context of high-risk pregnancies. Methods: A descriptive cross-sectional correlational survey design was used. A convenience sample of 404 high-risk pregnant women from a maternity department at the National Guard Health Affairs hospital, in Jeddah completed three online scales: the Connor-Davidson Resilience Scale, the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Results: Most women (89.85%) had low resilience, while only 1.98% had high resilience. There was a strong negative correlation between resilience and depression (r = -0.81, p < 0.001) and between resilience and anxiety (r = -0.79, p < 0.001). Women with low resilience had higher levels of depression and anxiety than women with high resilience. Additionally, women with high-risk pregnancies who have higher levels of resilience are more likely to have normal vaginal delivery, to be employed, and to have fewer pregnancy complications than those who have lower levels of resilience Conclusion: Resilience is an important factor for the mental health of women with high-risk pregnancies. Interventions to enhance resilience may help reduce the psychological burden of high-risk pregnancies and improve maternal and fetal outcomes. Further research is needed to explore the causal mechanisms and the modifiable factors that influence resilience.
Keywords: Resilience, High-Risk pregnancy, Prenatal anxiety, Prenatal depression, Mental health
Introduction
Pregnancy is a transformative journey marked by profound physical, emotional, and psychological changes. For many women, it is a period of heightened emotional vulnerability, where feelings of anticipation and joy may coexist with concerns, stressors, and, for some, a heightened risk of developing mental health issues such as anxiety and depression. Among pregnant women, the prevalence of anxiety and depression has been estimated to be as high as 15-25% and 10-15%, respectively [1,2]. However, for women experiencing high-risk pregnancies(HRP), this vulnerability is significantly amplified [3]. Pre-existing physical or mental conditions can cause HRP or may arise as new complications during pregnancy [4]. HRP is prevalent worldwide, with rates ranging from 6 to 40.5%. The prevalence of HRP in Saudi Arabia differs from region to region as it was reported by Hafez, Dorgham, and Sayed [5] ranging from (46.3%) in Al-Khobar City, to 63.6% in Taief City. Woefully, HRP is responsible for the deaths of 800 pregnant women daily across the world [6].
High-Risk Pregnancies (HRP) encompass a variety of conditions that elevate the likelihood of adverse outcomes for both the pregnant woman and the fetus. Maternal age is a significant factor, with advanced maternal age, typically defined as 35 years or older at the time of delivery, associated with increased risks of gestational diabetes, preeclampsia, and chromosomal abnormalities [7]. Pre-existing medical conditions, such as hypertension, diabetes, heart disease, autoimmune disorders, renal disease, and respiratory conditions, can complicate pregnancy and heighten the risk of adverse outcomes [8]. Moreover, women with a history of previous pregnancy complications, including preterm birth, fetal growth restriction, placental abnormalities, recurrent miscarriages, or stillbirths, are considered at higher risk for experiencing similar complications in subsequent pregnancies [9]. Multiple gestation pregnancies, such as twins, triplets, or higher-order multiples, are inherently high-risk due to an increased likelihood of preterm birth, low birth weight, gestational diabetes, preeclampsia, and other complications associated with carrying multiple fetuses [10]. Placental abnormalities, including placenta previa, placental abruption, and placenta previa, can lead to significant maternal and fetal complications, including bleeding and preterm birth [11]. Genetic factors also play a role, with certain genetic conditions or chromosomal abnormalities in either the mother or the fetus increasing the risk of pregnancy complications and adverse outcomes [12].
In addition, Maternal lifestyle factors, such as substance abuse (including tobacco, alcohol, and illicit drugs), inadequate nutrition, and obesity, are associated with increased risks of pregnancy complications such as preterm birth, fetal growth restriction, and birth defects [13]. Psychosocial factors, including socioeconomic disadvantage, limited access to healthcare, intimate partner violence, and mental health disorders such as depression and anxiety, can negatively impact maternal and fetal health outcomes [14].
Moving from all traditional HRP to pregnancies conceived through Assisted Reproductive Technologies (ART), such as In Vitro Fertilization (IVF), Intracytoplasmic Sperm Injection (ICSI), and ovulation induction, may be at increased risk for complications such as multiple gestation, preterm birth, and birth defects [15]. Additionally, other obstetric complications such as gestational diabetes, gestational hypertension, preeclampsia, intrauterine growth restriction, preterm labor, and fetal anomalies detected on prenatal screening or diagnostic tests, contribute to the complexity of high-risk pregnancies [16].
Consequently, HRP is associated with increased uncertainty, mental strain, and distress [13, 14]. Studies indicate a high prevalence of mental disorders among those with HRP, including depression (22.7–36.6%), anxiety (17.3–27.3%), and stress (19.8–31.7%) [17]. Negative emotions during pregnancy may also lead to risky decisions, with research suggesting an elevated risk of suicide among women facing HRP [17]. The physical, mental, and social consequences of HRP collectively impact the well-being of affected women [18]. Prenatal anxiety and depression are not only distressing for the expectant mother but also have far-reaching implications. They are associated with adverse perinatal outcomes, including preterm birth, low birth weight, and developmental problems in the child [17, 18]. Therefore, understanding the factors that may mitigate the impact of high-risk pregnancy on maternal mental health is of utmost importance [19].
Resiliency, in the context of psychological well-being, refers to an individual’s ability to adapt and bounce back from adversity. Research has suggested that resilient individuals may possess coping strategies and social support systems that enable them to withstand stressors and maintain psychological well-being, even in the face of high-risk circumstances [20, 21]. However, despite the growing interest in resiliency as a protective factor in prenatal mental health, there is a noticeable gap in the literature concerning its specific role among high-risk pregnant women. Understanding how resiliency influences the prevalence and severity of prenatal anxiety and depression in this population is critical for several reasons. Firstly, uncovering the relationship between resiliency and mental health outcomes in high-risk pregnancies can guide the development of targeted interventions and support systems tailored to the unique needs of these women. Such interventions could not only alleviate maternal suffering but also potentially improve birth outcomes, thus reducing the burden on healthcare systems [22]. Secondly, this research can contribute to the broader understanding of resiliency as a dynamic psychological construct, shedding light on its modulatory effects in the context of pregnancy. It can help elucidate whether resiliency acts as a buffer against the detrimental effects of high-risk pregnancy on maternal mental health and whether it fosters more adaptive coping strategies [7,23].
The prevalence of high-risk pregnancies in Saudi Arabia varies depending on the criteria and the population studied. Some of the factors that may contribute to high-risk pregnancies include maternal age, parity, gestational diabetes, preeclampsia, and restless legs syndrome. Accordingly, Fayed et al. [24] investigated the impact of maternal age on pregnancy outcomes in Saudi Arabia and found that 14.4% of the women had high-risk pregnancies. They also reported that adolescents and older mothers had increased risks of preterm delivery, gestational diabetes, and cesarean section [24]. Moreover, Rajbanshi et al. [25] examined the association between risk stratification and severe maternal morbidity in Nepal and found that women with high-risk pregnancies were 4.2 times more likely to develop severe maternal morbidity conditions during childbirth. They used the Malaysian antenatal risk stratification approach, which applies four color codes based on maternal past and present medical and obstetric risk factors [25].
Additionally, Almalki et al. [26] assessed the knowledge of obstetric danger signs among Saudi Arabian women and found that 70% of the participants knew at least one of these three danger signs during the antenatal period: vaginal bleeding, severe headache, and reduced fetal movement. They also found that women with higher education, higher income, and previous exposure to health education had better knowledge of obstetric danger signs [26]. Moving to another study conducted by Almeneessier et al. [27] estimated the prevalence of restless legs syndrome among pregnant women in Saudi Arabia and found that it was 18.9%. They also reported that restless legs syndrome was associated with an increased risk of preterm delivery, low birth weight, and cesarean section [27]. In conclusion, as the number of high-risk pregnancies continues to rise due to various factors, including maternal age and medical complexities, it becomes increasingly important to explore potential protective factors that can enhance the psychological well-being of these expectant mothers. Therefore, a comprehensive understanding of this relationship can inform the development of targeted interventions and support systems to improve the mental health and overall well-being of high-risk pregnant women, potentially leading to better maternal and neonatal outcomes in this vulnerable population.
The significance of the study:
The study delves into the intricate dynamics between resiliency and prenatal mental health within the context of high-risk pregnancies, aiming to yield significant contributions across various domains. Pregnancy constitutes a period marked by heightened emotional vulnerability, where expectant mothers may grapple with a spectrum of emotions ranging from anticipation and joy to stress and apprehension [1, 2]. In the realm of high-risk pregnancies, which encompass conditions posing threats to both maternal and fetal well-being, the challenges are further compounded by the need for heightened medical surveillance and interventions [4]. Consequently, expectant mothers facing high-risk pregnancies are particularly susceptible to psychological distress, including anxiety and depression, with adverse implications extending to perinatal outcomes such as preterm birth and low birth weight [2, 10].
In this context, understanding the protective role of resiliency assumes paramount importance, yet there exists a notable gap in the literature regarding its specific influence among high-risk pregnant women. This research endeavors to address this gap by elucidating how resiliency shapes the prevalence and severity of prenatal anxiety and depression, offering valuable insights that can inform the development of tailored interventions and support programs. By enhancing maternal well-being and potentially mitigating adverse perinatal outcomes, these insights hold implications not only for expectant mothers but also for healthcare providers, policymakers, and society at large. This study underscores the significance of integrating resiliency-focused approaches into prenatal care for high-risk pregnancies, ultimately striving to foster a supportive and empowering environment for expectant mothers facing heightened challenges during this critical phase of their lives [4, 10].
Theoretical framework:
A possible theoretical framework for the study aims to examine the relationships between high-risk pregnancy (HRP), resilience, and prenatal anxiety and depression. HRP is the independent variable, which refers to any condition that may endanger maternal or fetal health during pregnancy. Resilience is the mediator variable, which refers to the ability to cope with and adapt to stress and adversity. Prenatal anxiety and depression are the dependent variables, which refer to the emotional distress experienced by pregnant women.
The transactional version of stress and Coping (Lazarus & Folkman [28] in the context of a high chance of being pregnant (HRP), posits that strain arises from the interplay between the pregnant woman and her surroundings. This version emphasizes cognitive appraisal, in which individuals compare the importance of stressors and investigate their potential to cope with them. Resilience, as a mediator variable on this take a look at, performs an important role in influencing how pregnant girls appraise and deal with the strain of HRP. Higher ranges of resilience are related to extra adaptive coping techniques and higher mental health consequences.
By integrating the Transactional version of stress and Coping, the objective is to explore how pregnant ladies perceive and respond to the strain of HRP, with selected attention on the position of resilience in shaping their coping mechanisms and mental fitness consequences. Conservation of assets theory (Hobfoll [29] idea indicates that strain occurs when individuals understand the danger or loss of valued assets. Resilience is conceptualized because of the availability and mobilization of those resources, which could buffer the effect of stressors. Inside the context of HRP, pregnant girls may additionally enjoy a depletion of assets which includes bodily health, social guidance, and resilience.
Resilience serves as a shielding thing by assisting girls to preserve and refill those assets, thereby mitigating the poor consequences of stress on mental health.via making use of the Conservation of assets concept, the take look seeks to examine how pregnant women get admission and how utilization of resources influences their ability to deal with the demanding situations of HRP and save the development of prenatal anxiety and depression.
The Biopsychosocial model of Perinatal mental fitness [Dunkel Schetter & Tanner [30] The Biopsychosocial model integrates biological, mental, and social elements that affect the mental health of pregnant girls and their infants. Resilience is recognized as a defensive factor inside this model, contributing to fantastic maternal and little one outcomes. Within the context of HRP, the Biopsychosocial model emphasizes the complicated interaction among organic factors (e.g., maternal health fame), mental elements (e.g., coping mechanisms), and social elements (e.g., social assist networks) in shaping maternal intellectual health outcomes. By employing the Biopsychosocial version, the study aims to explain how resilience interacts with numerous biopsychosocial elements to influence the revel in of strain and coping amongst pregnant women facing HRP.In precis, this expanded framework elucidates the pathways through which resilience mediates the relationship between HRP and prenatal anxiety and depression, drawing on key concepts from every theoretical version to look at hypotheses and analysis.
Aim of the study:
The current study aimed to investigate the relationship between resiliency and the prevalence and severity of prenatal anxiety and depression in the context of high-risk pregnancies. More specifically the study looked at the following:
• Assess the level of resilience, depression, and anxiety, among high pregnancies women.
• Find the association between, resilience, depression, and anxiety, among high-risk pregnant women.
• Examine the correlation between the demographic background of the participants and the level of resilience, and prenatal depression and anxiety among high-risk pregnancies
Hypothesis:
• Null Hypothesis (H0): There is no significant relationship between resiliency levels and the prevalence and severity of prenatal anxiety and depression among high-risk pregnant women.
• Alternative Hypothesis (H1): There is a significant negative relationship between resiliency levels and the prevalence and severity of prenatal anxiety and depression among high-risk pregnant women. Specifically, higher levels of resiliency are associated with lower rates of prenatal anxiety and depression in this population.
Methodology
Research Design
A descriptive cross-sectional correlational survey design was used to achieve the objectives of the current study. The design is considered appropriate since it can assess the score of resilience, depression, and anxiety, among high-risk pregnancies.
Research Setting and Participants: The current study included all high-risk pregnant women living in Jeddah, Saudi Arabia, and attending outpatient maternity clinics at the Ministry of National Guard Hospital at King Abdulaziz Medical City in the period between 2022 -and 2023 This hospital is a military tertiary facility that offers several healthcare services, with a capacity of 764 beds, catering to the medical needs of the Saudi Arabian population in the Western Region. According to the nurses’ managers of the maternity department and units, in 2022, the number of Inpatient Admissions was 21686, while the number of Outpatient Visits was 181613. Additionally, hospitalization for uncontrolled high-risk pregnant women is done in Obstetric Ward (1), which serves the antenatal patients, has a bed capacity of 25 beds, and operates 24/7, with an average of 47 antenatal admissions per month.
Sampling technique:
A convenient sampling technique was used to include (404) high-risk pregnant women living in Saudi Arabia and attending outpatient maternity clinics in the period between 2022 and 2023, and willing to participate and match the inclusion criteria which were any pregnant woman who was diagnosed as high-risk pregnancy having serious conditions such as diabetes, hypertension, preeclampsia, etc., able to read and write, and agree to provide informed consent to participate in the web-based form survey.
Sample size calculation:
The cumulative admissions in the outpatient maternity department and specifically in ward 1 amounted to 182177 cases during the period of data collection (2022-2023). Subsequently, utilizing the Rao-soft calculation sample Size Calculator by Raosoft, Inc. [31] the determined sample size for the cross-sectional survey was 384 participants. This sample size was deemed sufficient, adhering to the recommended criteria of a 95% confidence level and a 5% margin of error.
In terms of the numbers, you selected above, the sample size n and margin of error E are given by
x=Z(c/100)2r(100-r)
n=Nx/((N-1)E2+x)
E=Sqrt[(N-n)x/n(N-1)]
Where N is the population size, r is the fraction of responses that you are interested in, and Z(c/100) is the critical value for the confidence level c.
Tools of the study
To achieve the objectives of the current study 4 tools will be used as follows:
1. Demographic background: this part was used to question the participants about their age, marital status, level of education, health income, occupation, number of children, reproductive and gestational history, etc.
2. The Arabic version of the 10-item Connor-Davidson Resilience Scale [32] (CD-RISC-10)
The Connor-Davidson Resilience Scale (CD-RISC-10) is a shortened version of the original CD-RISC, comprising 10 statements that assess different facets of resilience. It primarily measures an individual's hardiness, encompassing qualities like flexibility, self-efficacy, emotional regulation, optimism, and cognitive focus under stress. Respondents rate each item on a five-point scale, ranging from 0 (not at all true) to 4 (true nearly all the time), resulting in a total score between 0 and 40. Higher scores indicate greater resilience, while lower scores suggest less resilience or difficulty in bouncing back from challenges.
Interpreting CD-RISC-10 scores involves quartile-based categorization. The lowest quartile, with scores ranging from 0 to 29, signifies the lowest resilience, while the second quartile spans scores between 30 and 32. The third quartile falls between scores of 33 and 36, and the top quartile includes scores from 37 to 40. Lower scores in the lowest or second quartile may indicate challenges in coping with stress and adversity.
Regarding the scale's validity and reliability, the CD-RISC-10 has undergone extensive validation. According to the Connor-Davidson manual (24), all versions of the resilience scales have been validated and are valuable in different contexts. However, the CD-RISC-10 stands out for its robust validity, reliability, and practicality. Additionally, a study conducted by Aloba et al. (25) tested the scale among student nurses in Southwestern Nigeria and found that it demonstrated adequate reliability, with a Cronbach's alpha of .81, and satisfactory validity, showing significant correlations with measures of self-esteem, depression, religiosity, and psychological distress.
3. Arabic version of Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9, developed by Kroenke, Spitzer, & Williams [33] in 2001, is a versatile tool used for various purposes including screening, diagnosing, monitoring, and measuring the severity of depression. It consists of nine questions, and the total score is obtained by adding up the scores for each question. The scoring system assigns values of 0, 1, 2, and 3 to the response categories "not at all," "several days," "more than half the days," and "nearly every day," respectively.
Interpreting the PHQ-9 score is based on cut points: scores of 5, 10, 15, and 20 represent thresholds for mild, moderate, moderately severe, and severe depression, respectively. In other words, a score of 0-5 indicates mild depression, 6-10 suggests moderate depression, 11-15 signifies moderately severe depression, and 16-20 represents severe depression. Question 9 in the PHQ-9 assesses suicide risk with a single screening question. A positive response to this question indicates the need for further assessment of suicide risk by a qualified professional.
The PHQ-9's diagnostic validity has been demonstrated in studies conducted in primary care and obstetrical clinics. Scores greater than 10 on the PHQ-9 exhibit a sensitivity of 88% and a specificity of 88% for identifying Major Depressive Disorder. Psychometric properties such as reliability and validity are robust, with high internal consistency, as indicated by Cronbach's alphas of .86 and .89 in different patient populations. Additionally, criteria validity was established through structured interviews conducted by mental health professionals.
4. Arabic version of Generalized Anxiety Disorder 7-item (GAD-7)
The Generalized Anxiety Disorder 7-item (GAD-7) is a widely used self-report questionnaire developed by Kroenke, Spitzer, & Williams [34] in 2001 to screen for Generalized Anxiety Disorder (GAD) and assess the level of anxiety in individuals over the past 2 weeks. This tool consists of seven items that inquire about various aspects of anxiety, including feeling nervous or on edge, inability to control worrying, excessive worry about different things, difficulty relaxing, restlessness, irritability, and feelings of impending danger. To assess anxiety severity, respondents rate their symptoms on a scale of 0 to 3, with 0 being "not at all," 1 indicating "several days," 2 representing "more than half the days," and 3 signifying "nearly every day." A total score is calculated by summing the scores for each item, resulting in a range of 0 to 21. A score of 8 or higher is often used as a cut-off to identify probable cases of generalized anxiety disorder, indicating the need for further diagnostic assessment. This cut-off demonstrates a sensitivity of 92% and specificity of 76% for diagnosing GAD.
Moreover, the GAD-7 allows for the categorization of anxiety severity as follows: scores of 0-4 indicate mild anxiety, while scores of 5-9 suggest moderate anxiety. Recent research, such as a meta-analysis by Plummer et al. [35] in 2016, supports the use of a cut-off score of 8 to optimize sensitivity without compromising specificity. The GAD-7 has shown acceptable psychometric validity in various populations, including test-retest reliability, diagnostic validity, convergent validity, factorial validity, and internal consistency [36]. In addition, a study on university students in Saudi Arabia found good internal consistency of the GAD-7, as measured by Cronbach's alpha (0.80) [37].
Data Collection Procedure:
Once the official permission to conduct the study was obtained from King Abdullah International Medical Research Center’s (KAIMRC) and Institutional Review Boards (IRB), the data collection process was started. A link to an interactive Arabic version of 10- the item resilience scale. Next, participants were offered to take a second survey on their anxiety (generalized anxiety disorder 7 questionnaires (GAD7))9 and depression (patient health questionnaire 9 (PHQ9). The study was advertised through, (1) the researchers’ social networks, including emails to colleagues in the King Saud University campus including the three regions; (2) social media; and (3) organizational mailing lists. The participants were asked to sign the informed consent before filling out the questionnaires of the survey.
Data Management and Analysis Plan
The data were coded and analyzed using SPSS's version 23. Data were presented using descriptive statistics for discrete variables in the form of frequencies and percentages and interval and ratio variables in the form of means and standard deviations. The regression model was used to elicit the association between the key dependent variable which is either a dichotomized measure of meeting screening levels of GAD and depression (binary logistic regression); or continuous GAD7 and PHQ2 score (linear regression). Participants’ sociodemographic and scores of resiliencies depression, and anxiety were analyzed using the Pearson r test to find the association between study variables. The significance level will be at p<0.05.
Ethical Considerations:
An official approval from KAIMRC and IRB (No. NRJ21J/251/10) was received. In addition, written consent was obtained from all participants. Subjects were informed that their participation in the study was voluntary, and they could withdraw without any penalty at any time. They were assured that their answers were kept anonymous during the study and that their data was kept confidential. Additionally, at the time of data collection, the researchers ensured the anonymity, confidentiality, and privacy of the participants ‘responses throughout the research study.
Results
Presents (Table 1) the demographic profile of women at high risk of pregnancy. The average age of the women in the study was 29.9 years, with a standard deviation of 8.7. Notably, a significant proportion of participants (34.7%) fell within the age range of 20 to 25 years, indicating a relatively young cohort. The majority of participants (64.1%) had completed secondary school, emphasizing the importance of educational background in understanding mental health outcomes. Furthermore, a substantial number of women (36.6%) were unemployed, highlighting a potential socioeconomic factor that may contribute to the overall well-being of high-risk pregnant women.
| Demographic Characteristics | F | % |
|---|---|---|
| Mean age (years) | 29.9 ± 8.7 years | |
| Range | 34 years | |
| Age grouping | ||
| 20 -25 years | 143 | 34.70% |
| 26-30years | 140 | 35.30% |
| 31-40 years | 58 | 14.40% |
| More than 40years | 63 | 15.60% |
| Level of education | ||
| Illiterate | 87 | 21.50% |
| Read &write | 30 | 7.5 0 % |
| Secondary school | 259 | 64.10% |
| High level (bachelor) | 28 | 6.90% |
| Job | ||
| Working | 256 | 63.40% |
| Not working. | 148 | 36.60% |
Table 1: Distribution of Demographic Characteristics among High-risk Pregnancy Women (n=404)
Provides (Table 2) insights into the obstetric history of high-risk pregnant women. A significant majority (81.2%) had a parity of less than three, indicating that a considerable portion of the participants were in the early stages of their reproductive history, possibly experiencing their first or second pregnancy. Additionally, almost two-thirds (59.9%) had a gravidity of fewer than three, further emphasizing the prevalence of women in the early stages of their reproductive journey. The high prevalence of pregnancy-related issues, such as anemia (24.3%) and hypertension (27.0%), underscores the complexity of health considerations in high-risk pregnancies.
| Obstetric History | Studied Women (n=404) | |
|---|---|---|
| F | % | |
| Gravidity | ||
| § < 3 | 242 | 59.90% |
| § = 3 | 162 | 40.10% |
| Parity | ||
| § < 3 | 328 | 81.20% |
| § = 3 | 76 | 18.80% |
| Complications of the current pregnancy ((High risk pregnancy)) | ||
| Diabetes with pregnancy | 59 | 14.60% |
| Hypertension with pregnancy | 109 | 27.00% |
| bleeding in early pregnancy | 62 | 15.30% |
| placenta previa & bleeding in late pregnancy | 35 | 8.70% |
| Abnormal growth of the fetus | 41 | 10.10% |
| Anemia during pregnancy | 98 | 24.30% |
| Methods of delivery | ||
| § NVD | 114 | 28.20% |
| § Elective Caesarian Section (CS) | 242 | 59.90% |
| § CS after trial of NVD | 48 | 11.90% |
| Complications during current Labor | ||
| No complications | 62 | 15.30% |
| Intra-natal Hemorrhage | 47 | 11.70% |
| Laceration (cervical & vaginal) | 62 | 15.30% |
| Cervical dystocia | 57 | 14.10% |
| Maternal distress | 79 | 19.60% |
| Fetal heart rate abnormalities for baby | 97 | 24.00% |
| Duration of puerperium | ||
| From 2- 4 weeks | 220 | 54.50% |
| From 5-6 weeks | 93 | 24.00% |
| From 7-8 weeks | 91 | 22.50% |
Table 2: Obstetric History among High-Risk Pregnancy Women (n=404)
Displays (Table 3) the results of the Connor-Davidson Resilience Scale (CD-RISC-10) for women at high risk of pregnancy. The most prevalent responses for resilience were associated with the second and tenth questions, where "Rarely true" and "Sometimes true" were selected by 49.5% and 48.3% of the women, respectively.
| (CD-RISC-10) items: | Not true at all (0) | Rarely true (1) | Sometimes true (2) | Often true (3) | True nearly all the time (4) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | F | % | F | % | |
| I can adapt when changes occur . | 1 | 0.20% | 181 | 44.10% | 153 | 37.30% | 51 | 12.40% | 18 | 4.40% |
| I can deal with whatever comes my way. | 113 | 27.60% | 203 | 49.50% | 63 | 15.40% | 25 | 6.10% | 0 | 0.00% |
| I try to see the humorous side of things when I am faced with problems. | 128 | 31.20% | 123 | 30.00% | 85 | 20.70% | 68 | 16.60% | 0 | 0.00% |
| Having to cope with stress can make me stronger. | 1 | 0.20% | 84 | 20.50% | 174 | 42.40% | 91 | 22.20% | 54 | 13.20% |
| I tend to bounce back after illness, injury, or other hardships. | 0 | 0 | 127 | 31.00% | 147 | 35.90% | 87 | 21.20% | 43 | 10.50% |
| I believe I can achieve my goals, even if there are obstacles. | 3 | 0.7 | 99 | 24.10% | 180 | 43.90% | 90 | 22.00% | 32 | 7.80% |
| Under pressure, I stay focused and think clearly. | 1 | .2%0 | 117 | 28.50% | 180 | 43.90% | 71 | 17.30% | 35 | 8.50% |
| I am not easily discouraged by failure. | 5 | 1.20% | 98 | 23.9 | 180 | 43.90% | 86 | 21.00% | 35 | 8.50% |
| I think of myself as a strong person when dealing with life’s challenges and difficulties. | 0 | 0.00% | 103 | 25.10% | 161 | 39.30% | 95 | 23.20% | 45 | 11.00% |
| I can handle unpleasant or painful feelings like sadness, fear, and anger. | 0 | 0.00% | 101 | 24.60% | 198 | 48.30% | 75 | 18.30% | 28 | 6.80% |
Table 3: Connor-Davidson Resilience Scale (CD-RISC-10) Among High-risk pregnancy Women (n=404)
Illustrates (Figure 1) the distribution of resilience levels among women facing high-risk pregnancies. The majority of women (89.85%) fell into the lowest resilience quartile, whereas the smallest percentage (1.98%) was found in the third quartile of the resilience scale.
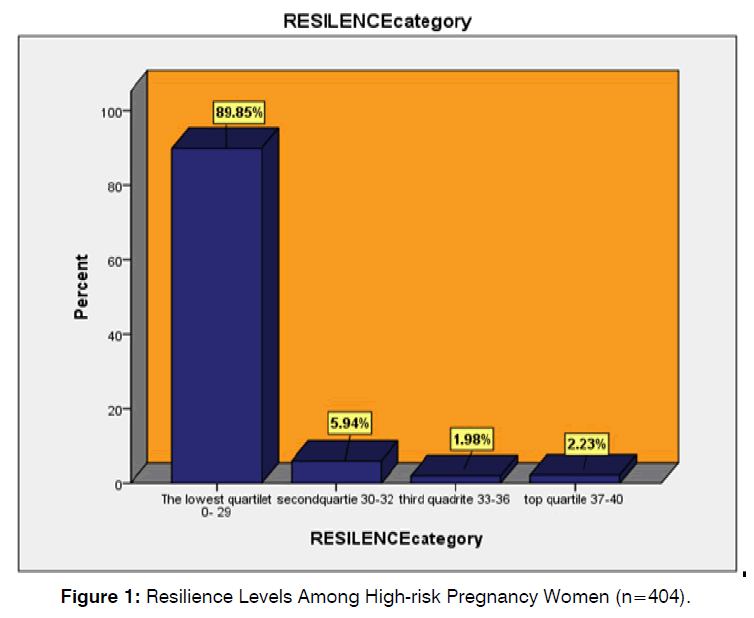
Figure 1: Resilience Levels Among High-risk Pregnancy Women (n=404).
Presents (Table 4) the Patient Health Questionnaire (PHQ-9) Depression scales for women at high risk of pregnancy. Among those with pregnancy complications, only one woman (0.2%) reported experiencing suicidal thoughts nearly every day.
| (PHQ-9) items | (Not at all)(0) | Several Days(-1) | More than half the days(-2) | Nearly every day (-3) | ||||
|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | F | % | |
| 1. Little interest or pleasure in doing things | 4 | 1 | 170 | 41.5 | 183 | 44.6 | 47 | 11.5 |
| 2. Feeling down, depressed, or hopeless | 1 | 0.2 | 112 | 27.3 | 241 | 58.8 | 50 | 12.2 |
| 3. Trouble falling or staying asleep, or sleeping too much | 1 | .2 0 | 118 | 28.8 | 169 | 41.2 | 116 | 28.3 |
| 4. Feeling tired or having little energy | 2 | .5 0 | 134 | 32.7 | 206 | 50.2 | 62 | 15.1 |
| 5. Poor appetite or overeating | 0 | 0 | 174 | 42.4 | 191 | 46.6 | 39 | 9.5 |
| 6. Feeling bad about yourself or that you are a failure or have let yourself or your family down | 0 | 0 | 292 | 71.2 | 100 | 24.4 | 12 | 2.9 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0 | 0 | 60 | 14.6 | 342 | 83.4 | 2 | 0.5 |
| 8. Moving or speaking so slowly that other people could have noticed. or the opposite being so fidgety or restless that you have been moving around a lot more than usual | 0 | 0 | 154 | 37.6 | 228 | 55.6 | 22 | 5.4 |
| **9. Thoughts that you would be better off dead, or of hurting yourself Thoughts that you would be better off dead, or of hurting yourself | 359 | 87.60% | 35 | 8.50% | 9 | 2.20% | 1 | 0.2 |
Table 4: Patient Health Questionnaire (PHQ-9) Depression Scales Among High-risk Pregnancy Women (n=404)
Depicts (Figure 2) the levels of depression among women facing high-risk pregnancies. Among all the women, 5% experienced moderate to severe depression (scores 6–10), while more than three-quarters (83.20%) had moderate to moderate-severe depression (scores 8–15).
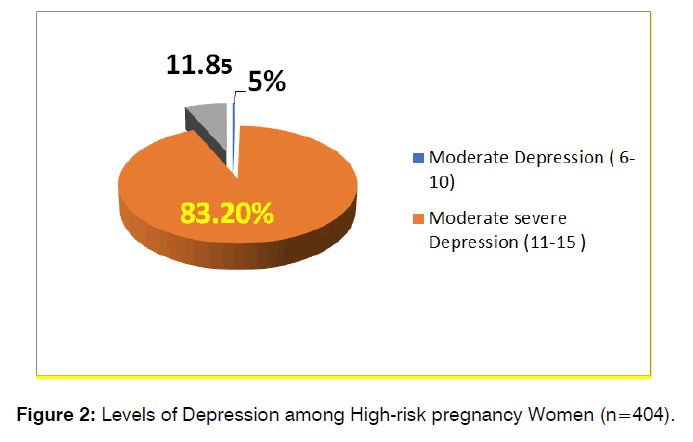
Figure 2: Levels of Depression among High-risk pregnancy Women (n=404).
Focuses (Table 5) on Generalized Anxiety Disorder 7-item (GAD-7 Anxiety) among women facing high-risk pregnancies. About one-third (29.8%) of the women indicated that they experienced excessive worry about various things. Additionally, more than half of the women (56.1%) reported having difficulty relaxing for more than half of the days. Moreover, a substantial majority (65.9%), equivalent to two-thirds of the women, reported experiencing feelings of nervousness, anxiety, or being on edge.
| (GAD) items: | (Not at all true)(0) | Several Days(-1) | More than half days(-2) | Nearly every day(-3) | ||||
|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | F | % | |
| 1. Feeling nervous, anxious, or on edge | 0 | 0 | 270 | 65.9 | 135 | 32.9 | 0 | 0 |
| 2. Not being able to stop or control worrying | 78 | 19 | 209 | 51 | 118 | 28.8 | 0 | 0 |
| 3. Worrying too much about different things | 0 | 0 | 92 | 22.4 | 191 | 46.6 | 122 | 29.8 |
| 4. Trouble relaxing | 0 | 0 | 175 | 42.7 | 230 | 56.1 | 0 | 0 |
| 5. Being so restless that it is hard to sit still | 20 | 4.9 | 242 | 59 | 143 | 34.9 | 0 | 0 |
| 6. Becoming easily annoyed or irritable | 0 | 0 | 167 | 40.7 | 227 | 55.4 | 11 | 2.7 |
| 7. Feeling afraid as if something awful might happen | 195 | 47.6 | 156 | 38 | 54 | 13.3 | 0 | 0 |
Table 5: Generalized Anxiety Disorder 7-item (GAD-7 Anxiety) Among High-risk Pregnancy Women (n=404)
Discloses (Figure 3) the levels of anxiety among women facing high-risk pregnancies. More than half of the women (52.7%) experienced moderate to moderate-severe anxiety, while the smallest percentage (0.3%) reported severe anxiety.
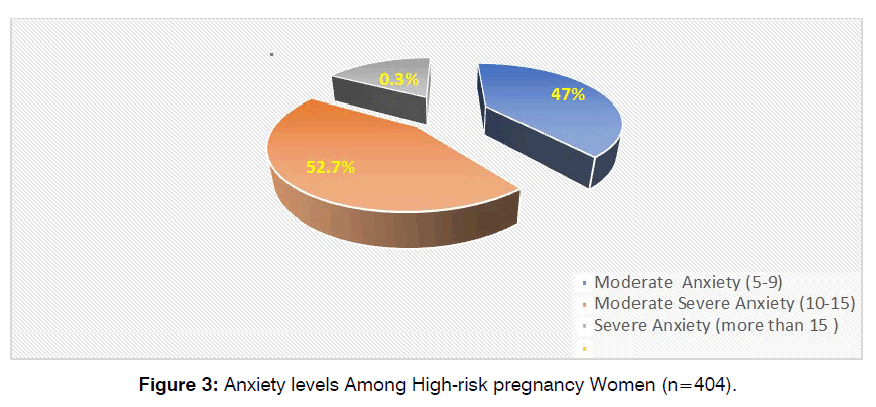
Figure 3: Anxiety levels Among High-risk pregnancy Women (n=404).
Indicates (Table 6) significant associations between depression levels and resilience levels, as well as between depression levels and total generalized anxiety disorder (GAD) levels. The chi-square tests demonstrate that these variables are not independent.
| Depression levels | Resilience levels | X2 P | |||
|---|---|---|---|---|---|
| The lowest quartile 0- 29 | Second quartile 30-32 | Third quartile 33-36 | Top quartile 37-40 | ||
| Moderate depression (6-10) | 24 | 5 | 0 | 1 | X2 =33.984a P=.000** |
| 6.60% | 20.80% | 0.00% | 11.10% | ||
| Moderately severe depression (11-15) | 280 | 10 | 3 | 3 | |
| 77.10% | 41.70% | 37.50% | 33.30% | ||
| Severe depression (16-20) | 59 | 9 | 5 | 5 | |
| 16.30% | 37.50% | 62.50% | 55.60% | ||
| Total | 363 | 24 | 8 | 9 | |
| 100.00% | 100.00% | 100.00% | 100.00% | ||
| Total Generalized Anxiety Disorders levels: | X2 =19.069a P.= .004** | ||||
| Moderate anxiety 5-9 | 170 | 12 | 2 | 6 | |
| 46.80% | 50.00% | 25.00% | 66.70% | ||
| Moderate severe anxiety 10-15 | 193 | 11 | 6 | 3 | |
| 53.20% | 45.80% | 75.00% | 33.30% | ||
| sever anxiety of more than 15 | 0 | 1 | 0 | 0 | |
| 0.00% | 4.20% | 0.00% | 0.00% | ||
| Total | 363 | 24 | 8 | 9 | |
| 100.00% | 100.00% | 100.00% | 100.00% | ||
Table 6: Relation between Resilience Levels GAD anxiety and Depression Among High-risk Pregnancy Women (n=404)
For depression levels and resilience levels: The chi-square test for the association between depression levels and resilience levels is significant (X2 = 33.984, p < 0.001), indicating that the two variables are not independent. The table shows that the proportion of women with moderate depression is higher in the second quartile of resilience (20.8%) than in the other quartiles (6.6%, 0%, and 11.1%). The proportion of women with moderately severe depression is higher in the lowest quartile of resilience (77.1%) than in the other quartiles (41.7%, 37.5%, and 33.3%). The proportion of women with severe depression is higher in the third and top quartiles of resilience (62.5% and 55.6%) than in the other quartiles (16.3% and 37.5%).
For depression levels and total GAD levels: The chi-square test for the association between depression levels and total generalized anxiety disorder (GAD) levels is also significant (X2 = 19.069, p = 0.004), indicating that the two variables are not independent. The table shows that the proportion of women with moderate anxiety is higher in the top quartile of resilience (66.7%) than in the other quartiles (46.8%, 50%, and 25%). The proportion of women with moderately severe anxiety is higher in the third quartile of resilience (75%) than in the other quartiles (53.2%, 45.8%, and 33.3%). The proportion of women with severe anxiety is higher in the second quartile of resilience (4.2%) than in the other quartiles (0%).
Presents (Table 7) the results of chi-square tests examining associations between resilience categories and various factors including job status, type of labor, and high-risk pregnancy complications. Significant associations were found between resilience categories and each of these factors, indicating that the variables are not independent. In terms of job status, a higher proportion of working women was observed in the lowest quartile of resilience, while non-working women were more prevalent in the top quartile. Regarding the type of labor, women with higher resilience levels were more likely to have had elective cesarean sections, while those with lower resilience levels were more likely to have had normal vaginal deliveries. Furthermore, the association between resilience categories and high-risk pregnancy complications was significant, with variations observed across resilience quartiles. For instance, women in the second quartile of resilience had higher proportions of diabetes with pregnancy, while those in the lowest quartile had higher proportions of hypertension with pregnancy and bleeding in early pregnancy. Conversely, women in the top quartile of resilience had higher proportions of anemia during pregnancy. These findings underscore the complex relationship between resilience and various pregnancy-related factors, highlighting the importance of considering resilience in the context of maternal health outcomes.
| Resilience Categories | Test P | ||||
|---|---|---|---|---|---|
| The lowest quartile 0-29 | Second quartile 30-32 | third quartile 33-36 | Top quartile 37-40 | ||
| Job | X2 = 20.194a P=.000** | ||||
| Working | 243 (66.9%) | 8 (33.3%) | 3 (37.5%) | 2 (22.2%) | |
| Not Working | 120 (33.1%) | 16 (66.7%) | 5 (62.5%) | 7 (77.8%) | |
| Total | 363 (100%) | 24 (100%) | 8 (100%) | 9 (100%) | |
| Type labor: | X2 =12.741a P= .047 | ||||
| NVD | 95 (26.2%) | 13 (54.2%) | 2 (25%) | 4 (44.4%) | |
| Elective CS | 224 (61.7%) | 9 (37.5%) | 6 (75%) | 3 (33.3%) | |
| CS After the trial of NVD | 44 (12.1%) | 2 (8.3%) | 0 (0.0%) | 2 (22.2%) | |
| Total | 363 (100%) | 24 (100%) | 8 (100%) | 9 (100%) | |
| High-risk pregnancy Complications: | X2 = 24.387a P = .05** | ||||
| Diabetes with pregnancy | 47 (12.9%) | 6 (25%) | 4 (50%) | 2 (22.2%) | |
| Hypertension with pregnancy | 105 (28.9%) | 3 (12.5%) | 0 (0.0%) | 1 (11.1%) | |
| Bleeding in early pregnancy | 58 (16%) | 4 (16.7%) | 0 (0.0%) | 0 (0.0%) | |
| Placenta previa& bleeding in late pregnancy | 32 (8.8%) | 2 (8.3%) | 1 (12.5%) | 0 (0.0%) | |
| Abnormal growth development of the fetus | 38(10.5%) | 2 (8.3%) | 0 (0.0%) | 1 (11.1%) | |
| Anemia during pregnancy | 83 (22.9%) | 7 (29.2%) | 3 (37.5%) | 5 (55.6%) | |
| Total | 363 (100%) | 24 (100%) | 8 (100%) | 9 (100%) | |
Table 7: The Correlation between Levels of Resilience, and Job, Type labor, & Pregnancy Complications among High-risk pregnancy Women
Shows (Table 8) the Pearson correlation coefficients between three psychological scales: Total Generalized Anxiety Disorder (GAD-7 Anxiety), Connor-Davidson Resilience Scale (CD-RISC-10), and Patient Health Questionnaire (PHQ-9) Depression Scales. The sample size (N) for all the correlations is 404, which is a relatively large and robust sample. The correlation coefficients range from -0.134 to 0.158, indicating weak linear relationships between the variables. The only statistically significant correlations (p < 0.01) are between GAD-7 Anxiety and PHQ-9 Depression (-0.134), and between CD-RISC-10 Resilience and PHQ-9 Depression (0.158). These correlations suggest that higher anxiety is associated with lower depression and higher resilience is associated with higher depression, but the effect sizes are small. The correlation between GAD-7 Anxiety and CD-RISC-10 Resilience is not statistically significant (p = 0.645), indicating no linear relationship between these variables.
| Items | Total Generalized Anxiety Disorder (GAD-7 Anxiety) | Connor-Davidson Resilience Scale (CD-RISC-10) | Patient Health Questionnaire (PHQ-9) Depression Scales | |
|---|---|---|---|---|
| Total Generalized Anxiety Disorder (GAD-7 Anxiety) | Pearson Correlation | 1 | 0.023 | 0.134** |
| Sig. (2-tailed) | 0.645 | 0.007 | ||
| N | 404 | 404 | 404 | |
| Connor-Davidson Resilience Scale (CD-RISC-10) | Pearson Correlation | 0.023 | 1 | 0.158** |
| Sig. (2-tailed) | 0.645 | 0.001 | ||
| N | 404 | 404 | 404 | |
| Patient Health Questionnaire (PHQ-9) Depression Scales | Pearson Correlation | 0.134** | 0.158** | 1 |
| Sig. (2-tailed) | 0.007 | 0.001 | ||
| N | 404 | 404 | 404 |
Table 8: Correlation among Total Generalized Anxiety Disorder (GAD-7 Anxiety), Connor-Davidson Resilience Scale (CD-RISC-10) and Patient Health Questionnaire (PHQ-9) Depression Scales, & Among High-risk pregnancy Women (n=404)
Shows (Table 9) the regression analysis table showcases models that predict anxiety and depression scores based on the resilience category. The first anxiety model indicates that the resilience category does not have a significant impact on anxiety scores (p = 0.820). However, the second anxiety model suggests a positive effect (p < 0.001), indicating that the resilience category has a significant impact on anxiety scores. In both depression models, the resilience category significantly predicts depression scores (p < 0.001). The Beta coefficient in the second anxiety model is standardized and indicates a moderate positive relationship between the resilience category and anxiety scores. Overall, the findings suggest that resilience has varying impacts on anxiety and depression, with depression showing higher effects in both models.
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p | 95.0% Confidence Interval for B | |||
|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Lower Bound | Upper Bound | ||||
| 1 | (Constant) | 9.613 | 0.138 | 69.9 | <0.001 | 9.343 | 9.883 | |
| RESILENCE category | 0.024 | 0.106 | 0.011 | 0.227 | 0.82 | -0.185 | 0.233 | |
| 1 | (Constant) | 13.04 | 0.245 | 53.14 | <0.001 | 12.558 | 13.522 | |
| RESILENCE category | 0.781 | 0.19 | 0.201 | 4.113 | <0.001 | 0.408 | 1.154 | |
Table 9: Regression analysis models for dependent variables (Anxiety and Depression) and independent variables (Resiliency) among high-risk pregnant women N=404
The scatter plot shows that both total anxiety and total resilience are significant predictors of total depression among high-risk pregnancy women, after controlling for each other. Total anxiety hurts total depression, while total resilience has a positive effect on total depression. The constant term is also significantly different from zero, indicating that there is a baseline level of total depression that is not explained by the independent variables (Figure 4).
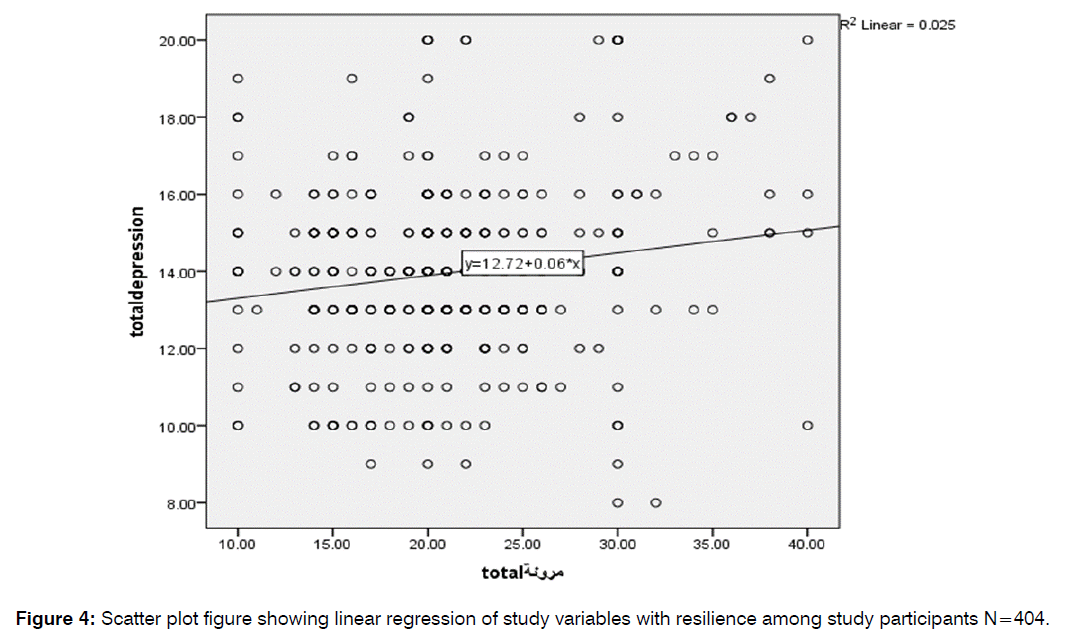
Figure 4: Scatter plot figure showing linear regression of study variables with resilience among study participants N=404.
Discussion
This study examined how High-Risk Pregnancy (HRP), resilience, and prenatal mental health are related. HRP is a condition that puts the mother or the baby at risk during pregnancy. Prenatal mental health is the emotional well-being of pregnant women [7]. The study found that women with High-Risk Pregnancies (HRP) had low resilience, high depression, and high anxiety, which may adversely affect maternal and fetal outcomes [38]. Resilience was negatively associated with depression, suggesting that it can buffer the negative effects of HRP on prenatal mental health [39]. The finding that 89.85% of the women fell into the lowest resilience quartile indicates that they have limited resources and support to cope with the stressors associated with HRP [40]. This may be due to factors such as adverse childhood experiences, lack of social support, low socioeconomic status, or previous trauma [10, 41]. Low resilience may also increase the risk of developing depression and anxiety, which are common mental health problems among women with HRP [39]. Depression and anxiety can impair maternal-fetal attachment, increase the risk of preterm birth, and affect postnatal bonding and infant development [42, 43].
The finding that resilience was negatively associated with depression supports the notion that resilience can protect against the development of mood disorders in the face of stress [44, 45]. Resilience may also moderate the impact of depression on maternal-fetal attachment, as women with higher resilience may be able to maintain a positive and nurturing relationship with their unborn child despite their depressive symptoms [46]. Resilience may therefore be a key factor for enhancing prenatal mental health and well-being among women with HRP.
The results also showed that resilience was associated with some demographic and pregnancy-related variables, such as age, education, marital status, parity, gestational age, and type of HRP. These associations may reflect the influence of various factors on resilience, such as life experience, social support, coping skills, and perceived control [47, 48]. These factors may also affect the perception and appraisal of HRP, and the ability to cope with its challenges and uncertainties [10, 20]. The effect of sociocultural factors on prenatal anxiety and depression is a crucial area of research. A comprehensive review discusses how pregnancy and childbirth are strongly linked to cultural factors It was emphasized that a woman’s experiences during pregnancy and childbirth are shaped by her cultural context. Cultural rituals, traditions, and practices associated with the perinatal period significantly influence mental health outcomes. The study also examines the influence of culture on psychopathology, help-seeking behaviors, and explanatory models of illness [49]. Another meta-analysis conducted by Insan et al. [50] including 34 studies involving 27,379 women assessed the social determinants linked to antenatal depression and anxiety among women in Bangladesh, India, and Pakistan. The analysis revealed significant associations between antenatal depression/anxiety and factors such as intimate partner violence, unplanned pregnancy, male gender preference, and poor relationships with in-laws. Additionally, the majority of studies (14 out of 34) indicated a trend showing a higher risk of antenatal depression/anxiety with increasing maternal age. Conversely, there was a trend suggesting that women with lower levels of education/literacy had reduced odds of experiencing antenatal depression/anxiety. While discussing depression and anxiety, this study emphasizes the relevance of cultural factors. It reviews risk factors and highlights the need to consider both categorical and continuous measures of mental health during pregnancy [51]. These studies collectively underscore the importance of sociocultural factors in shaping perinatal mental health outcomes. Cultural beliefs, social support networks, and stigma all play significant roles. Researchers continue to explore these aspects to enhance our understanding and improve support for safer pregnancy and birth outcomes.
Remarkably, the study revealed that women with HRP face considerable psychological challenges, such as low resilience, high depression, and high anxiety, which may have negative consequences for maternal and fetal health. Resilience was found to be a protective factor against depression and to be associated with various demographic and pregnancy-related variables. The study highlights the need for screening and intervention programs to identify and support women with HRP who are at risk of poor prenatal mental health, and to enhance their resilience and coping skills. The study also suggests that health care providers and policymakers should consider the psychosocial aspects of HRP, and provide adequate resources and support for women with HRP and their families.
Moreover, and moving to the linear regression analysis, the results of this study suggest that anxiety and resilience are important factors that influence the level of depression among high-risk pregnant women. Higher anxiety is associated with higher depression, while higher resilience is associated with lower depression. These findings are consistent with previous studies that have shown that anxiety and resilience are related to depression in pregnant women [52, 53]. Therefore Cognitive Behavioral Therapy (CBT)-Based Interventions and mindfulness activities, such as meditation and Mindfulness-Based Stress Reduction (MBSR) are effective in building resilience and are among resilience-enhancing interventions. This could be done by improving coping abilities, emotional regulation, self-awareness, and stress reduction [54] and the evidence-based research indicated that combining CBT and mindfulness provides a holistic approach to treating cognitive processes and emotional awareness simultaneously, leading to growth and courage. In addition, strong social interactions can build resilience by giving emotional affirmation, practical aid, and a sense of belonging [54].
Another evidence-based practices that enhance resilience is a healthy lifestyle comprising regular exercise, a balanced diet, and sufficient sleep is crucial for enhancing well-being and building resilience. To develop resilience, it's important to cultivate strengths, virtues, and positive emotions. The most effective way to achieve this is through psychoeducation and resilience training initiatives that teach stress management, coping mechanisms, and adaptive solutions. However, interventions tailored to individual requirements with evidence-based strategies and ongoing support are necessary for long-term effectiveness [55].
On the other hand, some studies have also reported contradictory results, such as no significant association between anxiety and depression [39] or a positive association between resilience and depression [48]. These discrepancies may be due to differences in the measurement, definition, or sample characteristics of anxiety, resilience, and depression [56]. Therefore, more research is needed to clarify the complex relationships among these psychological constructs in high-risk pregnancies.
Limitations of the Study
The study has some limitations that should be acknowledged. First, the sample size was relatively small and the participants were recruited from one hospital, which may limit the generalizability of the findings. Second, the study used self-report measures, which may be subject to bias and social desirability. To ensure the reliability of the study findings a sensitivity analysis was conducted to assess the robustness of our findings to potential biases. These analyses have allowed us to evaluate the consistency of results obtained from self-reported data and explore any discrepancies with objective measures where applicable. Despite these efforts, we recognize that our study is not without limitations. As highlighted in the manuscript, the reliance on self-reported data poses inherent challenges, and future research should aim to address these limitations through alternative methodologies or validation studies.
Third, the study was cross-sectional, which precludes causal inferences and temporal relationships. Future research should use larger and more diverse samples, include objective measures of HRP and prenatal mental health, and employ longitudinal designs to examine the changes and outcomes of resilience, depression, and anxiety throughout pregnancy and beyond.
Conclusion
The study’s results reveal the importance of resilience for the psychological and physical well-being of women with high-risk pregnancies. Resilience is associated with lower levels of depression and anxiety, which can adversely affect maternal and fetal health. The study suggests that interventions to enhance resilience may help reduce the negative effects of high-risk pregnancies on mental health outcomes. However, more longitudinal research is needed to confirm the causal role of resilience and to identify the factors that influence its development and expression. The study offers valuable insights for healthcare professionals and researchers who aim to support this vulnerable population.
Recommendations and Nursing Implications:
• Healthcare professionals should assess the resilience levels of women with high-risk pregnancies and provide them with appropriate resources and support to cope with the challenges and uncertainties of their condition.
• Screenings for depression and anxiety are crucial for pregnant women, along with necessary treatment and support. Building resilience in high-risk women during pregnancy can help reduce stress and depression while strengthening maternal-fetal attachment.
• Nurses should foster a trusting and empathetic relationship with women with high-risk pregnancies and help them identify and mobilize their personal and social strengths and resources.
• Interventions to enhance resilience should be tailored to the specific needs and preferences of each woman and should include strategies such as cognitive-behavioral therapy, mindfulness, positive psychology, coping skills, and peer support.
• Researchers should conduct more longitudinal studies to examine the effects of resilience on mental and physical health outcomes in women with high-risk pregnancies and their infants, as well as the mechanisms and moderators of these effects.
• Researchers should also explore the best ways to measure and operationalize resilience in this population and evaluate the effectiveness and cost-effectiveness of resilience-based interventions.
Acknowledgment
The researchers would like to acknowledge the support and cooperation of the participants who took part in this study. The researchers also expressed their gratitude to the supervisors of outpatients and ward 1 in the maternity department who facilitated the data collection process and provided the necessary resources for the study.
Conflict of Interest: All researchers affirm that they possess no conflicts of interest.
Funding Declaration: All authors state that this study has not received any financial support from either internal or external funding sources
References
- Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119(1-3):142-8..
- Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):8615.
- Li H, Bowen A, Bowen R, Muhajarine N, Balbuena L. Mood instability, depression, and anxiety in pregnancy and adverse neonatal outcomes. BMC Pregnancy Childbirth. 2021;21:1-9.
- Mirzakhani K, Khadivzadeh T, Faridhosseini F, Ebadi A. Development and psychometric evaluation of the High-Risk Pregnancy Well-Being Index in Mashhad: a methodological study. Reprod Health. 2022;19(1):218.
- Hafez SK, Dorgham LS, Sayed SA. Profile of high risk pregnancy among Saudi women in Taif-KSA. World J Med Sci. 2014;11(1):90-7.
- Liman I, Durojaiye K, Ezeike A, Amin MS, Mahmoud R, Babandi R. Maternal Mortality: A Two-Decade Review of Cases in a Tertiary Health Centre in Northcentral, Nigeria. Trop J Obstet Gynaecol. 2023;40(2):85-91.
- He J, Wang Y, Liu Y, Chen X, Bai J. Experiences of pregnant women with gestational diabetes mellitus: a systematic review of qualitative evidence protocol. BMJ Open. 2020;10(2):e034126.
- Yavas SP, Baysan C. Preterm labor conditions of women with high-risk pregnancy and related factors: a retrospective cohort study. J Ist Faculty Med. 2022;85(2):177-84.
- Smith MV, Gotman N, Yonkers KA, Lee H. The impact of psychiatric disorders on the quality of life of women during pregnancy. J Womens Health. 2019;28(1):12-234.
- Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):8615.
- Isaacs NZ, Andipatin MG. A systematic review regarding women’s emotional and psychological experiences of high-risk pregnancies. BMC Psychol. 2020;8:1-1.
- Monterrosa-Castro Á, Romero-Martínez S, Monterrosa-Blanco A. Positive maternal mental health in pregnant women and its association with obstetric and psychosocial factors. BMC Public Health. 2023;23(1):1013.
- Ramiro-Cortijo D, De la Calle M, Benitez V, Gila-Diaz A, Moreno-Jiménez B, Arribas SM, et al. Maternal psychological and biological factors associated to gestational complications. J Pers Med. 2021;11(3):183.
- Limouzin E, Beland J, Gauthier C, Herba C, Côté S, Janvier A, et al. Evaluation of a mental health promotion program (Ombrelles) in a high-risk pregnancy unit. Am J Obstet Gynecol. 2022;226(1):S620.
- Effati-Daryani F, Mohammad-Alizadeh-Charandabi S, Zarei S, Mohammadi A, Mirghafourvand M. Depression, anxiety and stress in the various trimesters of pregnancy in women referring to Tabriz health centres, 2016. Int J Cult Ment Health. 2018;11(4):513-21.
- Abera M, Hanlon C, Fedlu H, Fewtrell M, Tesfaye M, Wells JCK. Stress and resilience during pregnancy: A comparative study between pregnant and non-pregnant women in Ethiopia. PLOS Glob Public Health. 2023;3(5):e0001416.
- Van Haeken S, Braeken MA, Horsch A, Oosterman M, Bogaerts A. Development of a resilience-enhancing intervention during and after pregnancy: a systematic process informed by the behaviour change wheel framework. BMC Psychol. 2023;11(1):267.
- Akkineni R, Rao A, Ganjekar S. “Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services:” A Review. Indian J Soc Psychiatry. 2023;39(3):227-9.
- Alves AC, Cecatti JG, Souza RT. Resilience and stress during pregnancy: a comprehensive multidimensional approach in maternal and perinatal health. Sci World J. 2021;2021:1-7.
- Orri M, Gunnell D, Richard-Devantoy S, Bolanis D, Boruff J, et al. In-utero and perinatal influences on suicide risk: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(6):477-92.
- Holness N. High-risk pregnancy. Nurs Clin. 2018;53(2):241-51.
- Anhalt K, Telzrow CF, Brown CL. Maternal stress and emotional status during the perinatal period and childhood adjustment. Sch Psychol Q. 2007;22(1):74.
- Grussu P, Jorizzo GJ, Alderdice F, Quatraro RM. Preventing, Mitigating, and Treating Women’s Perinatal Mental Health Problems during the COVID-19 Pandemic: A Scoping Review of Reviews with a Qualitative Narrative Synthesis. Behav Sci. 2023;13(5):358.
- Seoud MA, Nassar AH, Usta IM, Melhem Z, Kazma A, Khalil AM. Impact of advanced maternal age on pregnancy outcome. Am J Perinatol. 2002;19(01):001-8.
- Rajbanshi S, Norhayati MN, Nik Hazlina NH. High-risk pregnancies and their association with severe maternal morbidity in Nepal: A prospective cohort study. PLoS One. 2020;15(12):e0244072.
- Maseresha N, Woldemichael K, Dube L. Knowledge of obstetric danger signs and associated factors among pregnant women in Erer district, Somali region, Ethiopia. BMC Women Health. 2016;16:1-8.
- Chen SJ, Shi L, Bao YP, Sun YK, Lin X, Que JY, et al. Prevalence of restless legs syndrome during pregnancy: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:43-54.
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer Sci Rev. 1984.
- Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. 1989;44(3):513.
- Schetter CD, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141-8.
- McCrum-Gardner E. Sample size and power calculations made simple. Int J Ther Rehabil. 2010;17(1):10-4.
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). J Anxiety Disord. 2003;18(2):76-82.
- Heritage B, Al Asadi AA, Hegney DG. Examination of the Connor-Davidson Resilience Scale 10 (CD-RISC-10) using the polytomous Rasch model. Psychol Assess. 2021;33(7):672.
- Aloba O, Olabisi O, Aloba T. The 10-item Connor–Davidson Resilience Scale: Factorial structure, reliability, validity, and correlates among student nurses in southwestern Nigeria. J Am Psychiatr Nurses Assoc. 2016;22(1):43-51.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-13.
- Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24-31.
- Doi S, Ito M, Takebayashi Y, Muramatsu K, Horikoshi M. Factorial validity and invariance of the 7-item generalized anxiety disorder scale (GAD-7) among populations with and without self-reported psychiatric diagnostic status. Front psychol. 2018;9:1741.
- Alghadir A, Manzar MD, Anwer S, Albougami A, Salahuddin M. Psychometric properties of the generalized anxiety disorder scale among Saudi University male students. Neuropsychiatr Dis Treat. 2020:1427-32.
- Redshaw M, Wynter K. Maternal mental health: Women’s voices and data from across the globe. BMC Pregnancy Childbirth. 2022;22(1):796.
- Tung I, Hipwell AE, Grosse P, Battaglia L, Cannova E, English G, et al. Prenatal stress and externalizing behaviors in childhood and adolescence: A systematic review and meta-analysis. Psychol Bull. 2023.
- Davis EP, Narayan AJ. Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Dev Psychopathol. 2020;32(5):1625-39.
- Wolf EJ, Logue MW, Hayes JP, Sadeh N, Schichman SA, Stone A, et al. Accelerated DNA methylation age: associations with PTSD and neural integrity. Psychoneuroendocrinology. 2016;63:155-62.
- Zhang X, Lou H, Tang X, Chen X. Socio-demographic characteristics and outcomes of pregnant women who delivered prior to and after the termination of the one-child policy in China: a comparative study. BMC Pregnancy Childbirth. 2021;21:1-8.
- Alves AC, Cecatti JG, Souza RT. Resilience and stress during pregnancy: a comprehensive multidimensional approach in maternal and perinatal health. Sci World J. 2021;2021:1-7.
- Armans M, Addante S, Ciciolla L, Anderson M, Shreffler KM. Resilience during pregnancy: How early life experiences are associated with pregnancy-specific stress. AARS. 2020;1:295-305.
- Smorti M, Ginobbi F, Simoncini T, Pancetti F, Carducci A, Mauri G, et al. Anxiety and depression in women hospitalized due to high-risk pregnancy: An integrative quantitative and qualitative study. Curr Psychol. 2023;42(7):5570-9.
- Mirzakhani K, Ebadi A, Faridhosseini F, Khadivzadeh T. Well-being in high-risk pregnancy: an integrative review. BMC Pregnancy Childbirth. 2020;20:1-4.
- Puertas-Gonzalez JA, Mariño-Narvaez C, Romero-Gonzalez B, Vilar-López R, Peralta-Ramirez MI. Resilience, stress and anxiety in pregnancy before and throughout the pandemic: a structural equation modelling approach. Curr Psychol. 2023;42(25):22013-23.
- Tung I, Hipwell AE, Grosse P, Battaglia L, Cannova E, English G, et al. Prenatal stress and externalizing behaviors in childhood and adolescence: A systematic review and meta-analysis. Psychol Bull. 2023.
- Insan N, Weke A, Forrest S, Rankin J. Social determinants of antenatal depression and anxiety among women in South Asia: A systematic review & meta-analysis. PLoS One. 2022;17(2):e0263760.
- Tikka SK, Thippeswamy H, Chandra PS. The Influence of Culture on Perinatal Mental Health. Infant Ment Health J. 2022;287-302.
- Evans J, Tiemeier H. Epidemiology of Prenatal Stress: Depression and Anxiety. Prenatal Stress Child Devel. 2021:13-9.
- Tuxunjiang X, Li L, Wumaier G, Zhang W, Sailike B, Jiang T. The mediating effect of resilience on pregnancy stress and prenatal anxiety in pregnant women. Front Psychiatry. 2022;13:961689.
- Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. 2018;8(6):e017858.
- Newman KM. Five science-backed strategies to build resilience. Greater Good Science Center, University of California, Berkeley, USA. 2016;9.
- Alves AC, Souza RT, Mayrink J, Galvao RB, Costa ML, Feitosa FE, et al. Measuring resilience and stress during pregnancy and its relation to vulnerability and pregnancy outcomes in a nulliparous cohort study. BMC Pregnancy Childbirth. 2023;23(1):396.
1King Saud Bin Abdul-Aziz University for Health Sciences, College of Nursing, Jeddah
2King Abdullah International Medical Research Center, Jeddah
3Professor of Psychiatric and Mental Health Nursing, Menoufia University, Egypt
4Assistant professor Nursing Oncology,College of Nursing ,Jeddah ,KSA
5Professor of Maternal and Newborn Health Nursing,Menoufyia University,Egypt.
Send correspondence to:
Amal I Khalil
Professor of Psychiatric and Mental Health Nursing, Menoufia University, Egypt, E-mail: khalila@ksau-hs.edu.sa
Paper submitted on March 1, 2024 and accepted on May 15, 2024
Citation: Amal I Khalil. High-Risk Pregnancy and Resilience: Unraveling the Links to Prenatal Anxiety and Depression. Int Tinnitus J. 2024;28(1):082-097.


