The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 24, Issue 2 / December 2020
Case Report Pages:92-95
10.5935/0946-5448.20200018
Perichondritis due to a herpes zoster Infection after an Ear Piercing: a Case Report
Authors: Ebrahim Karim, Setayesh Abazari,Sana Rashid, Mohammad Darvish
PDF
Abstract
Nowadays piercing has become one of the most popular fashionable and cultural customs and people of all ages are interested in this cosmetic procedure. One of the common sites of piercing is ears which, like any other piercing, can bring about many complications like infection, inflammation, allergic reaction, keloid formation, and traumatic tearing. In this paper, we report a case of perichondritis due to Staphylococcal secondary infection to a primary herpes zoster infection following ear piercing
Keywords: Otosclerosis- Ear piercing, perichondritis, herpes zoster, Staphylococcus aureus, case report
Introduction
Piercing has become very fashionable in last few decades. According to a study performed on 481 college students in New York, 42% of men and 60% of women have had their bodies pierced [1]. One of the most common sites of piercing is ears which, like any other piercing, can bring about many complications. Based on a study carried out in 1998, up to 35 percent of ear piercings caused at least one complication for the patient, ranging from minor infection (77 percent), allergic reaction (43 percent), and keloid formation (2.5 percent) to traumatic tearing (2.5 percent) [2]. Although these complications can be prevented, the risk surely augments if the procedure has been carried out by untrained personnel causing cartilage infection and perichondrial infection in which case should be treated as soon as possible [3-7]. In this paper we report a case of perichondritis due to Staphylococcal secondary infection to a primary herpes zoster infection following ear piercing.
Case Report
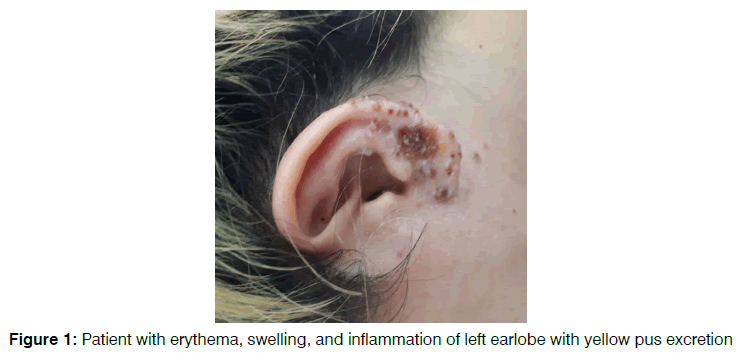
A 29-year-old woman was hospitalized due to erythema, swelling and inflammation of left earlobe with yellow pus excretion, alongside a severe pain in mandibular region. She gave a history of piercing her left ear about a month prior to the admission. As the signs firstly commenced about 2-week after piercing with erythema and inflammation of the earlobe, the patient visited a doctor and was treated initially with Coamoxiclav and Metronidazole for 10 days. For the signs started to worsen and a lesion emerged on the helix of the left ear, the patient was again visited by a doctor and a 12-day treatment with Cefazolin was prescribed. Yet, after using Cefazolin for 10 days, no sign of remission was observed. During a next visit 3 days before hospitalization, the patient was prescribed with Cloxacillin and Clindamycin. Since the signs continued to exist, the patient was admitted to the hospital. No previous history of neither diabetes nor collagen-vascular diseases was mentioned. Yet the patient mentions a history of migraine, cholestasis, appendectomy and a C-section surgery, none of which were recent. When admitted, the patient was being treated with Coamoxiclav (TID), Metronidazole 500mg (BID), 10 doses of Cefazolin 1g daily, cloxacillin 500mg (QID), clindamycin 300mg (TDS) and Mupirocin ointment.At the time of admission, the patient was conscious and stable. Vital signs were normal (blood pressure= 110 mmHg/ 80 mmHg, pulse rate=72 beats/min, respiratory rate=16 /min, oral temperature = 37'C). The left earlobe was erythematous, swollen and tender to touch. A lesion of about 0.1*0.5 cm was seen on the helix of the left ear. Cervical and posterior auricular lymph nodes were detectable and tender. There were no other symptoms found in physical examination. Laboratory studies showed: WBC=7100 /mm3, Hb=13.6 g/dl, Plt=305000 /mcL, Creatinine=0.7 mg/dl, Urea=16 mg/dl, Na=134 mEq/L, K=4 mEq/L, INR=1, PT=13sec. In audiometry test a decrease in hearing high-pitched sounds was detected. Based on signs, symptoms and culture taken from the yellow pus excreted from the lesion, the patient was diagnosed with perichondritis with Staphylococcal infection secondary to a herpes zoster infection.
Therefore, Prednizolon, Tavanex 750mg, Valaciclovir 500mg, and Diprotop ointment was prescribed. Two days after initiating the foresaid treatment, the lesion stop excreting and lymphadenopathy started to heal. Finally, the patient was discharged from the hospital and was prescribed to continue using Tavanex 750mg, Valaciclovir 500mg, and Diprotop ointment regularly and immediately refer to a doctor if any problem accured. Since there aren’t any records of patient's referral, we assume that the patient has been entirely treated Figure 1.
Figure 1: Patient with erythema, swelling, and inflammation of left earlobe with yellow pus excretion
Discussion
Nowadays piercing has become one of the most common fashionable and cultural customs and people of all ages are interested in this cosmetic procedure. But despite all the beauty benefits, it may come with lots of complications [8-10]. At the top of the list, infections are the most common complication that may occur. Other frequent complications are bleeding, metal allergy, tissue trauma, scarring, deformities, and other complications based on the implant material, site, sterilization and, other factors [8-12]. An Infection could occur in two situations: first in using inappropriate instrument and technique and second in poor care of wound and post piercing protection 13. Bacterial pathogens are more prevalent than viral and most reported cases declare Staphylococcus aureus, Pseudomonas aeruginosa, and Streptococcal species as a source of infection [14-18]. On the contrary, there are no firm reported cases of post piercing viral local infection although there are reported viral systemic infections especially viral hepatitis. Documents reveal that body piercing could be one of the transmission paths for the hepatitis B virus (HBV) and hepatitis C virus (HCV) [19-21]. Also, in 2009 Shaheen E Lakhan and Lindsey Harle reported a tongue piercing that comes with herpes simplex hepatitis which leads to fulminant hepatitis and at last death of the patient [22]. This case reported the first case of herpes zoster virus local infection and lymphadenopathy caused by ear piercing. Also, in this case there is a superinfection by Staphylococcus aureus. Staphylococcus aureus is a common pathogen in skin wound and injury since it is one of the skin microflora [23]. Also, bacterial superinfections, especially with Staphylococcus aureus, often happen after varicella infections due to damaged skin barrier and immunity [24, 25]. Although the patient has no complaints about hearing loss or tinnitus an audiometry test had been done to check out Ramsy hunt syndrome and results revealed a loss of hearing in the left ear. Ramsy hunt syndrome is a herpes neurological complication that happens when virus affects vestibulocochlear nerve and causes related signs including hearing loss, tinnitus, and vertigo. It also may cause facial nerve dysfunction and related sign and symptoms if it’s covered. Corticosteroids and antivirals are used to treat these features [26,27]. In this case, treatment should cover both viral (herpes zoster) and bacterial (Staphylococcus aureus) infection. For viral infection, acyclic nucleoside analogs including Acyclovir, Valacyclovir (acyclovir prodrug), Famciclovir (prodrug of Penciclovir) are suggested antiviral drugs. Since oral acyclovir bioavailability is not considerable, Valacyclovir and Famciclovir are the better choices in adult patients [28, 29].
Conclusion
For bacterial infection sufficient antibiotics according to the secretion smear, culture and patient age should be prescribed. At last, it is highly recommended to refer to a specialized center which observes hygienic standards to prevent serious complication and adverse events.
References
- Stirn A. Body piercing: medical consequences and psychological motivations. Lancet. 2003;361(9364):1205-15.
- Simplot TC, Hoffman HT. Comparison between cartilage and soft tissue ear piercing complications. American journal of otolaryngology. 1998;19(5):305-10.
- Cumberworth VL, Hogarth TB. Hazards of ear-piercing procedures which traverse cartilage: a report of Pseudomonas perichondritis and review of other complications. The British journal of clinical practice. 1990;44(11):512-3.
- Hanif J, Frosh A, Marnane C, Ghufoor K, Rivron R, Sandhu G. Lesson of the week: "High" ear piercing and the rising incidence of perichondritis of the pinna. Bmj. 2001;322(7291):906-7.
- Kent SE, Rokade AV, Premraj K, Butcher C. "High" ear piercing and perichondritis of the pinna. Bmj. 2001;323(7309):400.
- Widick MH, Coleman J. Perichondrial abscess resulting from a high ear-piercing--case report. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1992;107(6 Pt 1):803-4.
- Cossette JE. High ear-piercing. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1993;109(5):967-8.
- Van Hoover C, Rademayer CA, Farley CL. Body Piercing: Motivations and Implications for Health. Journal of midwifery & women's health. 2017;62(5):521-30.
- Kaatz M, Elsner P, Bauer A. Body-modifying concepts and dermatologic problems: tattooing and piercing. Clinics in dermatology. 2008;26(1):35-44.
- Breuner CC, Levine DA, Committee On A. Adolescent and Young Adult Tattooing, Piercing, and Scarification. Pediatrics. 2017;140(4).
- Fernandez AP, Neto IC, Anias CR, Pinto PCL, de Carvalho ECJ, Carpes AF. Post-piercing perichondritis. Brazilian journal of otorhinolaryngology. 2008;74(6):933-7.
- Holbrook J, Minocha J, Laumann A. Body piercing: complications and prevention of health risks. American journal of clinical dermatology. 2012;13(1):1-17.
- Messahel A, Musgrove B. Infective complications of tattooing and skin piercing. Journal of infection and public health. 2009;2(1):7-13.
- Manca DP, Levy M, Tariq K. Case Report: infected ear cartilage piercing. Canadian family physician Medecin de famille canadien. 2006;52:974-5.
- Weinberg JB, Blackwood RA. Case report of Staphylococcus aureus endocarditis after navel piercing. The Pediatric infectious disease journal. 2003;22(1):94-6.
- Rowshan HH, Keith K, Baur D, Skidmore P. Pseudomonas aeruginosa infection of the auricular cartilage caused by "high ear piercing": a case report and review of the literature. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2008;66(3):543-6.
- Staley R, Fitzgibbon JJ, Anderson C. Auricular infections caused by high ear piercing in adolescents. Pediatrics. 1997;99(4):610-1.
- Nnadozie UU, Ezeanosike OB, Maduba CC, Obu DC, Unigwe USD. Necrotizing soft tissue infection of both ear lobules occurring concomitantly in a set of twins following non-aseptic ear piercing: a case report. BMC pediatrics. 2020;20(1):54.
- Hayes MO, Harkness GA. Body piercing as a risk factor for viral hepatitis: an integrative research review. American journal of infection control. 2001;29(4):271-4.
- Tohme RA, Holmberg SD. Transmission of hepatitis C virus infection through tattooing and piercing: a critical review. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2012;54(8):1167-78.
- Yang S, Wang D, Zhang Y, Yu C, Ren J, Xu K, et al. Transmission of Hepatitis B and C Virus Infection Through Body Piercing: A Systematic Review and Meta-Analysis. Medicine. 2015;94(47):e1893.
- Lakhan SE, Harle L. Fatal fulminant herpes simplex hepatitis secondary to tongue piercing in an immunocompetent adult: a case report. Journal of medical case reports. 2008;2:356.
- Lee TC, Gold WL. Necrotizing Pseudomonas chondritis after piercing of the upper ear. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2011;183(7):819-21.
- Raulin O, Durand G, Gillet Y, Bes M, Lina G, Vandenesch F, et al. Toxin profiling of Staphylococcus aureus strains involved in varicella superinfection. Journal of clinical microbiology. 2010;48(5):1696-700.
- Aebi C, Ahmed A, Ramilo O. Bacterial complications of primary varicella in children. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1996;23(4):698-705.
- Sweeney C, Gilden D. Ramsay hunt syndrome. Journal of Neurology, Neurosurgery & Psychiatry. 2001;71(2):149-54.
- Monsanto RD, Bittencourt AG, Bobato Neto NJ, Beilke SC, Lorenzetti FT, Salomone R. Treatment and Prognosis of Facial Palsy on Ramsay Hunt Syndrome: Results Based on a Review of the Literature. International archives of otorhinolaryngology. 2016;20(4):394-400.
- Sauerbrei A. Varicella-zoster virus infections - antiviral therapy and diagnosis. GMS infectious diseases. 2016;4:Doc01.
- Gershon AA, Breuer J, Cohen JI, Cohrs RJ, Gershon MD, Gilden D, et al. Varicella zoster virus infection. Nature reviews Disease primers. 2015;1:15016.
1Department of Emergency Medicine, Besat Hospital, AJA University of Medical Sciences, Tehran, Iran
2Faculty of Medicine, Islamic Azad University, Tehran Medical Branch, Tehran, Iran.
3Department of Infectious Diseases and Tropical Medicine Research Center (IDTMRC), Department of Aerospace and Subaquatic Medicine, AJA University of Medical Sciences, Tehran, Iran
Send correspondence to:
Sana Rashidi
Department of Faculty of Medicine, Islamic Azad University, Tehran Medical Branch, Tehran, Iran, E-mail: drsanarashidi@yahoo.com Phone: +39 0649976808
Paper submitted on September 03, 2020; and Accepted on November 20, 2020
Citation: Perichondritis due to a herpes zoster Infection after an Ear Piercing: a Case Report. 24(2):92-95.