The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Medical and Hearing (Volume 28 S1) / March 2024
Research Article Pages:115-123
10.5935/0946-5448.2024.S1.19
Predictive role of IL-6 and NLR in screening Covid-19 patients with and without anosmia
Authors: Amer Salih Khalaf*, Ammar Mohammed Alwan, Maysam adnan mezher, Nada khaleel Yaseen, Rasheed Ali Rashid
PDF
Abstract
Background: In COVID-19 patients, a correlation was proposed between Neutrophil/Lymphocyte Ratio (NLR), IL-6 stages, and cytokine storm syndrome. Larger NLR and IL-6 concentrations are associated with faster case development and a greater likelihood of complications. However, the progression of the illness is milder in COVID-19 instances with anosmia. Objective: The objective of conducted research is detection predictive roles of IL-6 and Neutrophil/Lymphocyte Ratio (NLR) markers in screening Covid-19 sufferers with and without anosmia. Material and Methods: The present investigation was occurred at Salah Al-Din Teaching Hospital in Tikrit, Iraq for period; January- June of 2022. 90 nasopharyngeal swabs and blood samples were collected from individuals who visit to hospital after discovered them by the specialist physician. COVID-19 patients were divided into two groups based on the incidence of anosmia. 45 blood samples were harvested from healthy individuals that considered them as a control group. Ages of study groups ranged from 8 to 85 years old. Corona virus infection was detected by Polymerase Chain Reaction (PCR), NLR by Complete Blood Count (CBC) machine, and IL-6 by Sandwich-ELISA (Enzyme-Linked Immmunosorbent Assay) in study groups. Our results were analyzed by SPSS v. 23.0 and Graph pad prism v.6 statistical software programs. Results: Results of current study showed the age period 41-60 years scored highest percentages in all groups;(anosmia, without anosmia, and controls) while age period >80 scored lowest percentages in all groups with significant differences (p<0.5). Based on gender, males scored highest percentages in all groups than females with non-significant differences (p>0.05). Interleukin -6 (IL-6) scored significant (p<0.05) highest mean levels in patients without anosmia, followed by patients with anosmia, and then controls. On other hand, present investigation showed NLR scored statistical (p<0.05) highest mean levels in patients with anosmia, followed by patients without anosmia, and then controls. Receiver Operator Characteristic (ROC) curve results showed the IL-6 and NLR indicators scored statistically (p<0.05) highest sensitivity (91% and 84%) and specificity (100% and 81%) at cut off values (>38.5 and >1.87) in diagnosis patients without anosmia. In similarity, ROC curve results showed the IL-6 and NLR indicators scored significant (p<0.05) highest sensitivity (91% and 90%) and specificity (71% and 89%) at cut off values (>34.63 and >1.99) in detection patients with anosmia. Finally, pearson correlation coefficient results showed there is positive significant correlation (r= 0.769** and P<0.01**) between IL-6 and NLR markers in Covid-19 patients. Conclusions: Anosmia is positive correlate with age progression in Covid-19 patients. Levels of IL-6 and NLR markers are strong association with anosmia in patients. These markers can inserted within laboratory profile in diagnosis Covid-19 patients (with and without anosmia) due it have high sensitivity and specificity. Finally, there is positive correlation between IL-6 and NLR.
Keywords: Covid-19, IL-6, NLR, Anosmia, Olfactory Disorder.
Introduction
The coronavirus disease 2019 (COVID-19) first surfaced in Wuhan, China, in December of that year. It quickly spread over the entire globe and turned into a pandemic [1]. After then, an additional 6.8 million COVID-19 fatalities and over 759 million confirmed infections were recorded [2]. The respiratory tract, which includes are coughing, coryza, throat pain, breathing difficulties and hypoxemia, in addition to the overall inflammatory reaction, which includes fever and chills, discomfort, and exhaustion, are the signs and symptoms that are most common of COVID-19 [3].
According to Abdulhady et al. (2023), the neurotropic features of SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) can lead to neurological disorders such seizures, altered consciousness, and viral encephalitis. Anosmia and dysgeusia, the abrupt loss of senses of taste and smell, are among the neurological symptoms associated with SARS-CoV-2 [4]. A research by [5] on 347 COVID-19 patients found that 64.4% of the patients had impaired sense of smell. Women (72.4%) experienced smell disturbance more frequently than men (55.7%). According to [5], the start of olfactory indications may occur concurrently with, prior to, or following the emergence of other illness manifestations.
According to [6], age-related Olfactory Dysfunction (OD), neurological disorders, and nasal infections and inflammatory conditions may all be caused by destruction to the nose epithelium and the response of inflammatory cells. Subjects with COVID-19-related Olfactory Dysfunction (OD) were additionally found to exhibit changes in localized immunity in the olfactory area [7]. Nevertheless, the precise pathophysiological process responsible for COVID-19-induced Olfactory Dysfunction (OD) remains unclear.
According to [8], inflammation that is brought on by the body's immune system is crucial to the spread of virus. The neutrophil, leukocyte, and Neutrophil/Lymphocyte Ratio (NLR) rise in severe instances of immune system activation [9]. The relationship between these factors and the onset of neurological illness has not been well studied. In COVID-19 patients with neurological symptoms, found [10] substantially higher total neutrophil numbers and significantly fewer lymphocyte levels. An elevated NLR was linked to COVID-19-related discomfort in a different research [11].
In COVID-19, several investigations have revealed a similar tendency. A high NLR corresponds with intensity and advancement risk, according to 3 small Chinese studies conducted at the beginning of the pandemic [12]. This conclusion was supported by further research, which also revealed that the highest NLR is connected with ventilation that is mechanical and that an increasing trend is correlated with mortality [13]. NLR correctly assesses COVID-19 severity, according to a sizable meta-analysis involving 30 trials and 5570 individuals [14].
Interleukin-6, or IL-6, is a significant the Proinflammatory cytokine that is altered in bodily fluids over the course of several illnesses' establishment and incidence [15]. According to [16], IL-6 is thought to be one of the elements causing the cytokine storm among individuals with severe COVID-19. This might worsen the illness and raise the risk of consequences. As a result, it is often believed that the serum IL-6 level is a poor predictive indicator for COVID-19. The link between concentrations of IL-6 and Olfactory Disorder (OD) in individuals with COVID-19 wasn't consistently observed, despite evidence suggesting that IL-6 levels may have a role in the emergence of long-term Olfactory Disorder (OD) [17].
The objective of conducted research is detection predictive roles of IL-6 and Neutrophil/Lymphocyte Ratio (NLR) markers in screening Covid-19 sufferers with and without anosmia.
Materials and Methods
Samples collection: The present investigation was occurred at Salah Al-Din Teaching Hospital in Tikrit, Iraq for period; January- June of 2022, after obtaining the approval of the Ethics Committee from the Salah al-Din Health Directorate according to the administrative order No. (185/63/7) on 15/12/2021. 90 nasopharyngeal swabs (for diagnosis COVID-19 infection were approved by Polymerase Chain Reaction (PCR)) and blood samples were collected from individuals (EDTA and gel tube for detection NLR and IL-6 respectively) who visit to Salah Al-Din Teaching Hospital after discovered them by the specialist physician.
The criteria of the World Health Organization were relied upon in the clinical classification of patients according to the severity of the disease according to signs and symptoms.
The inclusion criteria were: patients with mild symptoms of Covid-19 infection without any sign of pneumonia, moderately infected patients with fever and pneumonia, both gender, and 18 years old and above.
Exclusion criteria were: patients with pre-existing olfactory problems of another cause, allergic rhinitis, sinusitis (chronic form), and severe Covid-19 infection with shortness of breath and severe hypoxia, as well as pregnant women, and less than 18 years old. Then COVID-19 patients were divided into two groups based on the incidence of anosmia. 45 blood samples were harvested from healthy individuals that considered them as a control group. Ages of study groups ranged from 8 to 85 years old.
Baselines data regarding age and gender were taken from each participant after informed consent was obtained from each one.
Methods: Collected nasopharyngeal swabs were used for diagnosis COVID-19 infection were approved by Polymerase Chain Reaction (PCR). The collected blood in EDTA tube was used for detection NLR in patients and controls by using Complete Blood Count (CBC) machine (Sysmex, Japan Company). While collected blood in gel tube was centrifuged by centrifuge machine (5000 rpm for 5 minutes) to have serum for measuring detection levels IL-6 by Sandwich-ELISA (Enzyme-Linked Immmunosorbent Assay) according to the instructions in the kit brochure (CUSBIO) in study groups.
Statistical analysis: IL-6 and NLR were showed as Mean± SD. ANOVA test was taken to detect variation significance among values of indicators within study groups. Gender and age periods characteristics were appeared like frequencies and percentages. The in similarities of percentages were measured by Pearson-Chi-square test. Receiver Operating Characteristic (ROC) curve was taken to scored Area under the Curve (AUC), cut off, sensitivity, and specificity of indicators. Pearson correlation coefficient used to detection type and strength of relationship between IL-6 and NLR indicators. Standard significant level was P≤0.05. SPSS v. 23.0 and Graph pad prism v.6 statistical software were taken to analyze current data.
Results
Demographic features of study groups: Results of current study showed the age period 41-60 years scored highest percentages in all groups; patients without and with anosmia (46.7% and 31.1%), as well as in controls (44.4%), while age period >80 scored lowest percentages in all groups; patients without and with anosmia (0.0% and 13.3%), as well as in controls (6.7%) with significant differences (p<0.5).
Based on gender, present outcomes showed the most participants were males; patients without and with anosmia (51.1% and 51.1%), as well as in controls (57.8%) with non-significant differences (p>0.05) Table 1.
| Number= 45 case for each group | Groups | Total | P value | ||||
|---|---|---|---|---|---|---|---|
| Without anosmia | With Anosmia | Control | |||||
| Jan-20 | n | 12 | 6 | 3 | 21 | P<0.05* | |
| % | 26.70% | 13.30% | 6.70% | 15.60% | |||
| 21-40 | n | 10 | 10 | 6 | 26 | P>0.05 | |
| % | 22.20% | 22.20% | 13.30% | 19.30% | |||
| Age groups (years) | 41-60 | n | 21 | 14 | 20 | 55 | P>0.05 |
| % | 46.70% | 31.10% | 44.40% | 40.70% | |||
| 61-80 | n | 2 | 9 | 13 | 24 | P<0.05* | |
| % | 4.40% | 20.00% | 28.90% | 17.80% | |||
| >80 | n | 0 | 6 | 3 | 9 | P<0.05* | |
| % | 0.00% | 13.30% | 6.70% | 6.70% | |||
| P value | P<0.001 | P>0.05 | P<0.001 | P<0.001 | |||
| *** | *** | *** | |||||
| Males | n | 23 | 23 | 26 | 72 | P>0.05 | |
| Gender | % | 51.10% | 51.10% | 57.80% | 53.30% | ||
| Females | n | 22 | 22 | 19 | 63 | P>0.05 | |
| % | 48.90% | 48.90% | 42.20% | 46.70% | |||
| P value | P>0.05 | P>0.05 | P>0.05 | P>0.05 | |||
Table 1. Distribution of study groups according to age groups and gender.
Levels of IL-6 and NLR within study groups: Present outcomes showed the IL-6 scored highest mean levels in patients without anosmia (93.61±29.28), followed by patients with anosmia (56.08±18.02), and then controls (22.98±8.40) with significant different (P<0.05) among all groups. Based on NLR, present investigation showed NLR scored highest mean levels in patients with anosmia (6.11 ±2.80), followed by patients without anosmia (3.76 ±0.94), and then controls (1.73±0.65) with significant different (P<0.05) among all groups Table 2 and Figure 1.
| N | Mean | SD | P value | ||
|---|---|---|---|---|---|
| Without anosmia | 45 | 93.61 a | 29.28 | ||
| IL-6 | With anosmia | 45 | 56.08 b | 18.02 | P<0.001*** |
| Control | 45 | 22.98 c | 8.4 | ||
| Without anosmia | 45 | 3.76 b | 0.94 | ||
| NLR* | With anosmia | 45 | 6.11 a | 2.8 | P<0.001*** |
| Control | 45 | 1.73 c | 0.65 | ||
Table 2. Distribution of study groups according to levels of IL-6 and NLR age groups and gender
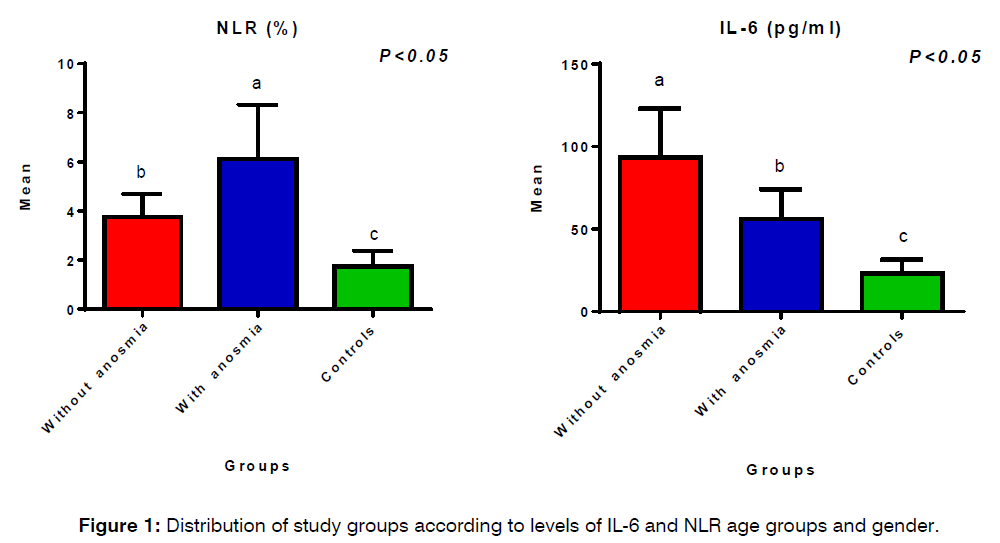
Figure 1: Distribution of study groups according to levels of IL-6 and NLR age groups and gender.
Receiver operator characteristic (ROC) curve of IL-6 and NLR markers: ROC curve results showed the IL-6 and NLR markers scored highest sensitivity (91% and 84%) and specificity (100% and 81%) at cut off values (>38.5 and >1.87) in detection patients without anosmia with important significant (p<0.05). In similarity, ROC curve results showed the IL-6 and NLR indicators scored highest sensitivity (91% and 90%) and specificity (71% and 89%) at cut off values (>34.63 and >1.99) in detection patients with anosmia with important significant (p<0.05) Table 3 and Figure 2.
| Without anosmia | ||||||
|---|---|---|---|---|---|---|
| With anosmia control | Area under curve(AUC) | Std. Error | P value | Cut-off | Sensitivity % | Specificity % |
| IL-6 | 0.96 | 0.022 | P<0.001*** | >38.5 | 91% | 100% |
| NLR | 0.804 | 0.048 | P<0.001*** | >1.87 | 84% | 81% |
| With anosmia | ||||||
| IL-6 | 0.911 | 0.031 | P<0.001*** | >34.63 | 91% | 71% |
| NLR | 0.918 | 0.036 | P<0.001*** | >1.99 | 90% | 89% |
Table 3: ROC curve, cut-off, sensitivity and specificity of IL-6 and NLR markers in screening study groups
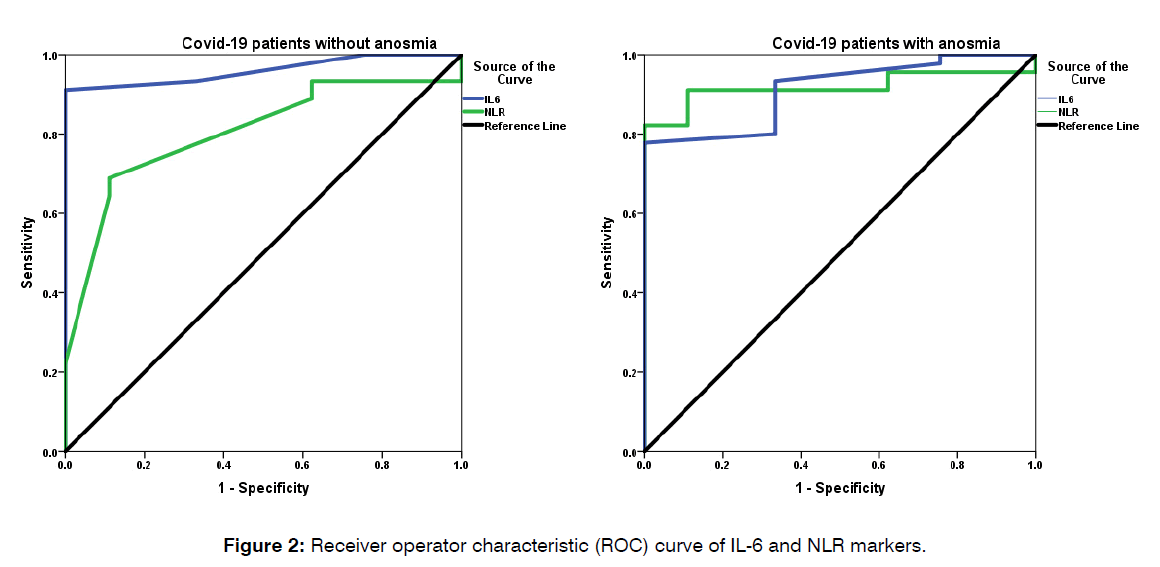
Figure 2: Receiver operator characteristic (ROC) curve of IL-6 and NLR markers.
Correlation relationship between IL-6 and NLR markers: As shown in Table 4 and Figure 3, pearson correlation coefficient results showed there is positive significant correlation ( r= 0.769 [** ]and P<0.01**) between IL-6 and NLR markers in Covid-19 patients Table 4 and Figure 3.
| IL-6 | ||
|---|---|---|
| NLR | Pearsoncorrelation coefficient (r) | 0.769** |
| Probability (P) value | P<0.01** | |
Table 4: Correlation relationship between IL-6 and NLR in Covid-19 patients
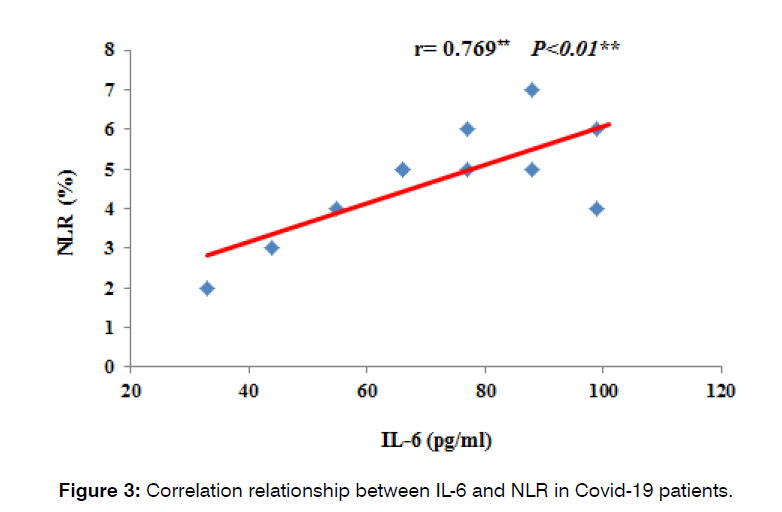
Figure 3: Correlation relationship between IL-6 and NLR in Covid-19 patients.
Discussion
Present investigation mentioned the most Covid-19 patients were with age groups >60 years, and these outcomes were matched with findings [18]. The average age of the study participants was 45.45±21.29 years. Our analysis revealed a mean age of 35.8 years, considerably greater than studies by [19] and [20], which reported a mean age of 36.5±13.9 years. The reality that the majority of these investigations were carried out during the early stages of the global outbreak, while the current study was carried out after the transmission network was confirmed, could assist in clarifying this age disparity.
He found [21] that patients over 65 had higher death rates, respiratory and extra pulmonary destruction of organs, and chronic inflammation, all of which enhanced their risk of contracting SARS-CoV-2. This result was consistent with present research. A further investigation conducted in Dubai discovered that older persons have COVID-19 at a seriousness that was 4.7 times greater compared to that of young people [22].
According to [4], females had a higher prevalence of Covid-19 infection (44.51%) than men (55.49%). These results differ from those of the current study, which found that males had a higher positive rate for Covid-19 infections (53.3%) than females (46.7%). According to [23], women's reproductive systems have higher amounts of ACE2, which makes them more susceptible to SARS-CoV-2.
Recently, He revealed [23] the death rate with Covid-19 infection occurred in older males due to have those patients’ chronic diseases, organ failure, and not efficient immune status.
He showed no association between age and anosmia, and these outcomes were matched with present outcomes.
According to our research, the rate of anosmia was comparable for male and female participants, which is inconsistent with findings by [3] that indicated a higher incidence of anosmia in female participants. Because the data was mostly based on self-reporting of indications, there may be memory bias as well as variations in methodology, symptom definition, demographic investigated, measuring tool, and other factors contributing to the disagreement in results among investigations. The research addresses biological variations in ACE receptor expression and X-chromosome position across gender as well as variations in initial smell as probable reasons for the higher frequency of these manifestations in females [8]. The SARS-CoV-2 entry requires the human cellular receptors ACE2 and TMPRSS2. The majority of these transmitters are found in the cells of the olfactory epithelium. Thus, the primary theory posits that anosmia results from injury to non-neuronal cells, which in turn impacts the regular metabolism of the olfactory system. A plausible rationale for the greater frequency seen in females might be because incomplete X chromosomal inactivation leads to elevated ACE2 expression [24] Table 1.
Outcomes of current investigation showed raised levels of NLR and IL-6 markers in Covid-19 patients versus controls, and these findings were matchers to results [25].
The emergence of COVID-19-related problems is attributed to the immunological reaction to the COVID-19 virus. Data points to a possible role for an unbalanced inflammation immune system in the onset of the disease's most dangerous phases. Consequently, adverse results in COVID-19 patients are linked to higher levels of circulatory mediators and reactants in the acute phase [25].
Numerous illnesses, notably COVID-19, have been linked to IL-6 [26]. It was shown that there is a substantial correlation between elevated levels of IL-6 and unfavorable clinical outcomes related to COVID-19, including ICU hospitalization, Acute Respiratory Distress Syndrome (ARDS), and mortality. Furthermore, compared to individuals with no complicated illness, individuals with such complex types of COVID-19 had blood IL-6 levels that were almost three times greater [27].
In addition to rising during the acute illness phase, an elevation in the amount of IL-6 constitutes one of the main causes of post-Covid-19 syndrome for four weeks following the initial infection [28]. Serum concentrations of IL-6 were shown to be considerably raised in patients following COVID-19 infection, regardless in the acutely or prolonged COVID-19 phase [28]. This finding suggests that heightened IL-6 is related with long COVID-19.
Olfactory disruption, encompassing both hyposmia and anosmia, is a commonly seen symptom of COVID-19. High amounts of the necessary receptors, such as ACE2, for SARS-CoV-2 entrance are expressed by nasal neuroepithelial cells [29]. Following the virus's entrance into the nasal neuroepithelial cells, an inflammatory reaction may result in abnormal neuronal function and olfactory disruption [30].
According to [31], Covid-19 patients with anosmia had higher levels of IL-6 than those lacking anosmia; however, our findings, which revealed higher concentrations of IL-6 in Covid-19 participants lacking anosmia compared to those with anosmia, were not consistent with their findings. There is proof that COVID-19 patients with anosmia had considerably lower blood IL-6 levels than those lacking anosmia. A milder course of the illness is being suggested for people who produce an effective antiviral defense on their olfactory epithelium, considered the initial line of barrier against virus infection. Nevertheless, olfactory disruption and a reduction in smell will occur due to the presence of the olfactory epithelium [32].
Participants with Olfactory Dysfunction (OD) have substantially higher levels of IL-6 in their mucus from the nose, the saliva, and plasma [33]. An examination of these alterations might link to systemic or localized inflammation, which could be the root cause or outcome of medical conditions associated with Olfactory Disorder (OD). Numerous investigations have revealed that IL-6 is crucial in the Olfactory Dysfunction (OD) that COVID-19 patient’s experience [34]. Yet, utilizing psychophysical olfactory ratings, the investigators were unable to find any association between Olfactory Disorder (OD) and Covid-19 [35]. The researchers postulated that because of immunology and inflammatory alterations, higher IL-6 levels may be a potential causative factor for the onset of Olfactory Disorder (OD) following a local or general infection [36].
A past investigation shown that, in comparison to individuals lacking Olfactory Disorder (OD), those suffering from Covid-19-related anosmia often had much lower blood levels of IL-6, and that these lower levels were associated with a gentler phase of the illness. It is possible to argue that anosmic patients with COVID-19 exhibit a milder condition due to their lower levels of IL-6 and cytokine storm [37].
Observations from [38] demonstrating higher NLR in Covid-19 patients compared to controls were consistent with our investigation. In patients with Covid-19, additional indicators of inflammation also rise dramatically along with the cytokines during the cytokine storm. Because neutrophils create reactive oxygen species which harm cell DNA, excessive inflammation brought on by Covid-19 seems to raise NLR levels [39]. Research has demonstrated the significance of the NLR level is a more accurate indicator of inflammation than the total counts of neutrophils and lymphocytes [40]. Inflammation causes neutrophilia, whereas immune system suppression causes lymphopenia. Both neutrophils and lymphocytes are engaged in the immunological response [41].
According to a prior investigation, the NLR is a useful indicator since it is necessary for clinical treatment and prognostic assessment of disease severity because it is elevated in Covid-19 participants and is linked to a greater risk of death [42].
According to a new study conducted among COVID-19 patients, an NLR value of 6.1 or more at the point of hospital stay was linked to severe illness, worsening clinical condition, and fatality. NLR incorporation as a predictive factor in COVID-19 prediction scales may enhance risk evaluation and direct suitable treatment plans for COVID-19 patients in addition to preparing for prospective viral pneumonias in the future [43].
According to [44], individuals who have anosmia had higher levels of NLR versus participants lack anosmia; these results were consistent with our own. According to earlier findings, having an elevated NLR was a reliable indicator of medical severity and an independent predictor of COVID-19 results (Yang et al., 2020). A 75-year-old man with COVID-19 who experienced acute stroke-like symptoms and signs had an elevated NLR, according to [10]. According to [45], in critically ill individuals with neurological diseases, the neutrophil count (NLR) were considerably greater while the lymphocyte count was decreased. An increase in neutrophils and a decrease in lymphocytes can both contribute to enhance NLR.
Recent study mentioned the increased levels of CRP, ESR, and NLR in patients with olfactory dysfunction suggest that they may play a role in the initiation of this symptom. Reduction of CRP and serum ferritin after 3 months from the onset of olfactory dysfunction can be a prognostic marker of smell recovery [46] Table 2.
According to the ROC curve, He found that [47] evaluation Covid-19 patients lacking anosmia resulted in moderate sensitivity (61%) and specificity (63%) of IL-6 at cut off >11.44. The results reported were lower than the current findings, which found that testing Covid-19 patients minus anosmia resulted in the highest sensitivity (91%) and specificity (100%) of IL-6 at cut off >38.5. According to [48], the authors found that patients with severe Covid-19 who live at high elevations may be distinguished between survivors and non-survivors using the IL-6 test.
ROC analysis was utilized to establish the threshold value of IL-6 level in predicting the severity and death from Covid-19. Prior ROC analysis showed that the cutoff values for both mortality and severity for IL-6 are larger than 50.27 and 120.83, respectively. The area under the ROC curve for IL-6 is 0.953 and 0.922, showing that it is a solid predictor for both conditions. According to [49], the degree of sensitivity and specificity readings for IL-6 for death and severity were 93.3% and 90.5%, respectively, and 90.0% and 86.7%, correspondingly.
Previous research demonstrated that because NLR has a moderate sensitivity (63%) and a good specificity (83%) at cut-off 7.02, it may be used as a medical laboratory prognostic indicator for death of Covid-19 patients lacking anosmia transferred to the intensive care unit [50]. The results we obtained, which demonstrated the best sensitivity (84%) and high specificity (81%) at cut-off >1.87, were favored above these findings.
The research team demonstrated that among COVID-19 patients, an NLR value of 6.1 or above at the point of hospitalization was linked to severe illness, worsening clinical condition, and fatality. NLR integration as a predictive factor in COVID-19 prognosis scales may enhance risk evaluation and direct suitable treatment plans for COVID-19 patients as well as for prospective viral pneumonias in the future [51].
With a cutoff threshold greater than 3.06, NLR may be a practical, affordable, and easy indicator to utilize for early COVID-19 infection patient prognosis. Aside from its cut-off point, NLR might be a reliable risk predictive in the identification of COVID-19 infections [52] Table 3.
He shown [53] that in individuals with both minor and severe Covid-19 illness, NLR and IL-6 correlated positively. These results complemented the current research. NLR and IL-6 have been found to be indicators of generalized inflammation and fatality risk factors in Covid-19 patients [54,55]. Accordingly, NLR and IL-6 may each function as a separate predictive biomarker for Covid-19 treatment [56].
Conclusion
Anosmia is positive correlate with age progression in Covid-19 patients. Levels of IL-6 and NLR markers are strong association with anosmia in patients. These markers can inserted within laboratory profile in diagnosis Covid-19 patients (with and without anosmia) due it have high sensitivity and specificity. Finally, there is positive correlation between IL-6 and NLR.
References
- Zumla A, Niederman MS. The explosive epidemic outbreak of novel coronavirus disease 2019 (COVID-19) and the persistent threat of respiratory tract infectious diseases to global health security. Curr Opin Pulm Med. 2020;26(3):193-6.
- Ghazizadeh M, Maleki M, Barati B, Ashjerdi MM. Association Between COVID-19 Severity and Olfactory Disturbance.
- Taha SI, Samaan SF, Ibrahim RA, El-Sehsah EM, Youssef MK. Post-COVID-19 arthritis: is it hyperinflammation or autoimmunity?. Eur Cytokine Netw. 2021;32(4):83-8.
- Abdelhady M, Husain MA, Hawas Y, Elazb MA, Mansour LS, Mohamed M, et al. Encephalitis following COVID-19 vaccination: a systematic review. Vaccines. 2023;11(3):576.
- Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. Jama. 2020;323(20):2089-90.
- Nikkhoo B, Mohammadi M, Hasani S, Sigari N, Borhani A, Ramezani C, et al. Elevated interleukin (IL)-6 as a predictor of disease severity among Covid-19 patients: a prospective cohort study. BMC. 2023;23(1):311.
- Ferdenzi C, Bousquet C, Aguera PE, Dantec M, Daudé C, Fornoni L, et al. Recovery from COVID-19-related olfactory disorders and quality of life: insights from an observational online study. Chem Senses. 2021;46:bjab028.
- Yin JX, Agbana YL, Sun ZS, Fei SW, Zhao HQ, Zhou XN, et al. Increased interleukin-6 is associated with long COVID-19: a systematic review and meta-analysis. Infect Dis Poverty. 2023;12(1):43.
- Rebholz H, Pfaffeneder-Mantai F, Knoll W, Hassel AW, Frank W, Kleber C. Olfactory dysfunction in SARS-CoV-2 infection: Focus on odorant specificity and chronic persistence. Am J Otolaryngol. 2021;42(5):103014.
- Asperges E, Albi G, Zuccaro V, Sambo M, Pieri TC, Calia M, et al. Dynamic NLR and PLR in predicting Covid-19 severity: A retrospective cohort study. Infect Dis Therapy. 2023;12(6):1625-40.
- Mohammed AK, Saber MM, Zaki ZM. Demographic data in COVID 19 patients. Minia J Med Res. 2023;34(1):126-32.
- Anupama A, Raman R, Ratheesh R, Palakkunnath S, Arumadi A, Ratheesh R. Symptomatology and Demographic Profile of COVID-19 Patients Admitted to a Tertiary Care Center in India: A Hospital Record-Based Study. Cureus. 2023;15(6).
- Kyala NJ, Mboya I, Shao E, Sakita F, Kilonzo KG, Shirima L, et al. Neutrophil-to-Lymphocyte Ratio as a Prognostic Indicator in COVID-19: Evidence from a Northern Tanzanian Cohort. MedRxiv. 2024:2024-02.
- Ahmed IM, Hefny HM, Ali AH, Refaie BM, Abdelal KM, Taha EM. Serum interleukin-6 as a predictor of the severity of coronavirus disease 2019. Res Opin Anaesth Intensive Care. 2023;10(1):68-74.
- Han H, Ma Q, Li C, Liu R, Zhao L, Wang W, et al. Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg Microbes Infect. 2020;9(1):1123-30.
- Wijeratne T, Sales CA, Crewther SG, Nguyen V, Karimi L. First Australian case of good recovery of a COVID-19 patient with severe neurological symptoms post prolonged hospitalization. Cureus. 2020;12(9).
- Statsenko Y, Al Zahmi F, Habuza T, Almansoori TM, Smetanina D, Simiyu GL, et al. Impact of age and sex on COVID-19 severity assessed from radiologic and clinical findings. Front Cell Infect Microbiol. 2022;11:777070.
- Ali FA, Jassim G, Khalaf Z, Yusuf M, Ali S, Husain N, et al. Transient anosmia and dysgeusia in COVID-19 disease: a cross sectional study. Int J Gen Med. 2023:2393-403.
- Sanli DE, Altundag A, Kandemirli SG, Yildirim D, Sanli AN, Saatci O, et al. Relationship between disease severity and serum IL-6 levels in COVID-19 anosmia. Am J Otolaryngol. 2021;42(1):102796.
- Talukder A, Razu SR, Alif SM, Rahman MA, Islam SM. Association between symptoms and severity of disease in hospitalised novel coronavirus (COVID-19) patients: a systematic review and meta-analysis. J Multidiscip Healthc. 2022:1101-10.
- Ganesh R, Grach SL, Ghosh AK, Bierle DM, Salonen BR, Collins NM, et al. The female-predominant persistent immune dysregulation of the post-COVID syndrome. Elsevier. 2022;97(3): 454-464.
- Bastug A, Bodur H, Erdogan S, Gokcinar D, Kazancioglu S, Kosovali BD, et al. Clinical and laboratory features of COVID-19: Predictors of severe prognosis. Int Immunopharmacol. 2020;88:106950.
- Fu J, Kong J, Wang W, Wu M, Yao L, Wang Z, et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China. Thrombosis Res. 2020;192:3-8.
- Sahin BE, Celikbilek A, Kocak Y, Koysuren A, Hizmali L. Associations of the neutrophil/lymphocyte ratio, monocyte/lymphocyte ratio, and platelet/lymphocyte ratio with COVID-19 disease severity in patients with neurological symptoms: A cross-sectional monocentric study. J Neurosci Rural Pract. 2023;14(2):224.
- Budu TE. Correlation of serum interleukin-6 levels and neutrophil-lympocyte ratio in the severity of COVID-19.
- Butowt R, Bilinska K, Von Bartheld CS. Chemosensory dysfunction in COVID-19: integration of genetic and epidemiological data points to D614G spike protein variant as a contributing factor. ACS Chem Neurosci. 2020;11(20):3180-4.
- Vélez-Páez JL, Baldeón-Rojas L, Cañadas Herrera C, Montalvo MP, Jara FE, Aguayo-Moscoso S, et al. Receiver operating characteristic (ROC) to determine cut-off points of clinical and biomolecular markers to discriminate mortality in severe COVID-19 living at high altitude. BMC. 2023;23(1):393.
- Chan AS, Rout A. Use of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19. J Clin Med. 2020;12(7):448.
- Hafez W, Nasa P, Khairy A, Jose M, Abdelshakour M, Ahmed S, et al. Interleukin-6 and the determinants of severe COVID-19: A retrospective cohort study. Medicine. 2023;102(45):e36037.
- Huang TB, Mao SY, Lu SM, Yu JJ, Luan Y, Gu X, et al. Predictive value of neutrophil-to-lymphocyte ratio in diagnosis of prostate cancer among men who underwent template-guided prostate biopsy: A STROBE-compliant study. Medicine. 2016;95(44):e5307.
- Făgărășan I, Rusu A, Comșa H, Simu TD, Vulturar DM, Todea DA. IL-6 and neutrophil/lymphocyte ratio as markers of ICU admittance in SARS-CoV-2 patients with diabetes. Int J Mol Sci. 2023;24(19):14908.
- Flores-Silva FD, Garcia-Grimshaw M, Valdes-Ferrer SI, Vigueras-Hernandez AP, Dominguez-Moreno R, Tristan-Samaniego DP, et al. Neurologic manifestations in hospitalized patients with COVID-19 in Mexico City. PLoS One. 2021;16(4):e0247433.
- Ghazizadeh M, Maleki M, Barati B, Ashjerdi MM. Association Between COVID-19 Severity and Olfactory Disturbance.
- Huang TB, Mao SY, Lu SM, Yu JJ, Luan Y, Gu X, et al. Predictive value of neutrophil-to-lymphocyte ratio in diagnosis of prostate cancer among men who underwent template-guided prostate biopsy: A STROBE-compliant study. Medicine. 2016;95(44):e5307.
- Jang SS, Pak KS, Strom A, Gomez L, Kim K, Doherty TA, et al. Pro‐inflammatory markers associated with COVID‐19‐related persistent olfactory dysfunction. Int Forum Allergy Rhinol. 2023.
- Liang Y, Mao X, Kuang M, Zhi J, Zhang Z, Bo M, et al. Interleukin-6 affects the severity of olfactory disorder: a cross-sectional survey of 148 patients who recovered from Omicron infection using the Sniffin’Sticks test in Tianjin, China. Int J Infect Dis. 2022;123:17-24.
- Kappelmann N, Dantzer R, Khandaker GM. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology. 2021;131:105295.
- Karimian A, Behjati M, Karimian M. Molecular mechanisms involved in anosmia induced by SARS-CoV-2, with a focus on the transmembrane serine protease TMPRSS2. Arch Virol. 2022;167(10):1931-46.
- Kouchek M, Aghakhani K, Memarian A. Demographic study of patients' mortality rate before and after the COVID‐19 outbreak: A cross‐sectional study. Health Sci Rep. 2024;7(2):e1845.
- Liu X, Wang H, Shi S, Xiao J. Association between IL-6 and severe disease and mortality in COVID-19 disease: a systematic review and meta-analysis. Postgrad Med J. 2022;98(1165):871-9.
- McCrae LE, Ting WT, Howlader MM. Advancing electrochemical biosensors for interleukin-6 detection. Biosens Bioelectron. 2023;13:100288.
- Mendonça CV, Mendes Neto JA, Suzuki FA, Orth MS, Machado Neto H, Nacif SR. Olfactory dysfunction in COVID-19: a marker of good prognosis?. Braz J Otorhinolaryngol. 2022;88:439-44.
- Nassar AA, Eltelety AM. Acute-phase reactants association with smell disorders in coronavirus disease 2019-infected patients. Pan Arab J Rhinol. 2023;12(2):2.
- Ramesh J, Reddy SS, Rajesh M, Varghese J. Evaluation of simple and cost-effective immuno-haematological markers to predict outcome in hospitalized severe COVID-19 patients, with a focus on diabetes mellitus-A retrospective study in Andhra Pradesh, India. Diabetes Metab Syndr Clin Res Rev. 2021;15(3):739-45.
- Ribeiro TF, Domingos CR, Rodrigues TD, Borin FH. Neutrophil-To-Lymphocyte Ratio (Nlr) In Covid-19 Patients. Hematol Transfus Cell Ther. 2023;45:S82.
- Ryu G, Kim DW. Th2 inflammatory responses in the development of nasal polyps and chronic rhinosinusitis. Curr Opin Allergy Clin Immunol. 2020;20(1):1-8.
- Santos HO, Delpino FM, Veloso OM, Freire JM, Gomes ES, Pereira CG. Elevated neutrophil-lymphocyte ratio is associated with high rates of ICU mortality, length of stay, and invasive mechanical ventilation in critically ill patients with COVID-19: NRL and severe COVID-19. Immunol Res. 2024;72(1):147-54.
- Seyfi S, Azadmehr A, Ezoji K, Nabipour M, Babazadeh A, Saleki K, et al. Mortality in ICU COVID-19 Patients Is Associated with Neutrophil-to-Lymphocyte Ratio (NLR): Utility of NLR as a Promising Immunohematological Marker. Interdiscip Perspect Infect Dis. 2023.
- Thomas R, John BM, Koothapally JT, Kumar S, Adiody S, Balachandran V, et al. Clinical and epidemiological spectrum of coronavirus disease 2019 in Central Kerala: a retrospective case series. Int J Comm Med Public Health. 2021;8(3):1503-7.
- Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163(1):3-11.
- Vaira LA, De Vito A, Deiana G, Pes C, Giovanditto F, Fiore V, et al. Correlations between IL-6 serum level and olfactory dysfunction severity in COVID-19 patients: a preliminary study. Eur Arch Otorhinolaryngol. 2022;279(2):811-6.
- Varghese B, Shajahan S, Anilkumar H, Haridasan RK, Rahul A, Thazhathedath H, et al. Symptomatology and epidemiologic characteristics of COVID 19 patients in Kerala, India. J Evol Med Dent Sci. 2020;9(46):3411-7.
- Wu J, Shen J, Han Y, Qiao Q, Dai W, He B, et al. Upregulated IL-6 indicates a poor COVID-19 prognosis: a call for tocilizumab and convalescent plasma treatment. Front Immunol. 2021;12:598799.
- Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504.
- Zeng F, Huang Y, Guo Y, Yin M, Chen X, Xiao L, et al. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis. 2020;96:467-74.
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33.
1Department of Otolaryngology, College of medicine, Tikrit University, Iraq
2Department of Clinical laboratory Sciences, College of Pharmacy, Tikrit University, Iraq
Send correspondence to:
Amer Salih Khalaf
Department of Otolaryngology, College of medicine, Tikrit University, Iraq, E-mail: Amer.s@tu.edu.iq
Paper submitted on March 04, 2024; and Accepted on March 22, 2024
Citation: Amer Salih Khalaf. Predictive role of IL-6 and NLR in screening Covid-19 patients with and without Anosmia. Int Tinnitus J. 2024;S1:115-123


