The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 20, Issue 1 / June 2016
Research Article Pages:11-17
10.5935/0946-5448.20160003
Preliminary longitudinal results of neuropsychological education as first and sole intervention for new tinnitus patients
Authors: Olav Victor Gerald Wagenaar; Marjan Wieringa; Lia Mantingh; Sophia E. Kramer; Rob Kok
PDF
Abstract
Introduction: Tinnitus is a potentially aggravating symptom without curative treatment. Cognitive Behavioral Therapy has been proved effective. It aims to learn to cope with tinnitus by reducing fearfull appraisal of tinnitus. Education is an important part of that therapy. Neuropsychological education alone in an early stage of the symptom might reduce the need for extensive therapy. Objective: To evaluate change of tinnitus related handicaps after neuropsychological education.
Materials and Methods: One hundred and six new tinnitus patients without otological ilnesses were educated in a neurophysiological model of tinnitus after otological inspection and audiometry. This was organized as a monthly standard session. Primary outcome was the Tinnitus Handicap Inventory (THI) score and subscores before intervention and 6 weeks after with follow up after 12 months. Seventy four participants were included for analysis.
Results: Six weeks post intervention a trend was seen in reduction of catastrophic reactions. After 12 months a significant decrease in THI scores was observed (all p values ≤ 0.01). The majority received no other treatment after the education. There were no significant differences between participants evaluating the workshop positively or negatively with respect to THI scores or tinnitus severity.
Conclusion: Neuropsychological education may be a sufficient intervention for new tinnitus sufferers.
Keywords: tinnitus, neuropsychology, education, counseling, disease prevention
Introduction
Chronic subjective tinnitus is a phantom sound perception that affects millions of people worldwide [1] . The burden of disease can vary greatly, from tinnitus without noticable suffering to very severe symptoms associated with the risk of suicide [2 - 4] . Having bothersome tinnitus is also associated with psychosomatic suffering [5,6] , depression, anxiety, irritability, sleep disturbance [7,8] , cognitive dysfunctioning [9,10] , general loss of fitness, loss of quality of life, higher health care consumption and loss of economic productivity [11] .
While neurostimulation and sound therapies are promissing, but still experimental [12,] there is no evidence from studies to show that farmacological or other medical interventions have (direct) positive effect in the treatment of tinnitus [13,14] . In the absence of a cure for tinnitus, clinical management typically focuses on coping by reducing the burden like distress, anxiety or depression and on the audiological treatment of hearing loss [12,15] .
Although cognitive behavioral therapy (CBT) has been proved to be an effective treatment [16] , Tinnitus Retraining Therapy (TRT) [17] provides the most widely used treatment for symptom management. In both CBT and TRT education has an important role. In TRT, directive counselling is combined with sound therapy using hearing aids (or if necessary cochlear implants), broad band ear-level sound generators or environmental sound enrichment (types of masking). A randomised controlled trial by Henry et al. [18] suggests that the combination of masking and counselling in TRT is more effective in establishing habituation than tinnitus masking alone [19] . The TRT protocol is fairly extensive in that it recommends follow up sessions at decreasing intervals during two years in which the counselling is repeated.
Objectives
How effective education is without any form of sound therapy or even without behavioral therapy, remains unclear. For sufferers aswell as caretakers, tinnitus is a complex phenomenon to cope with, which requires specialized knowledge. In the first period after the onset of symptoms, patients tend to seek information and guidance. General information is usually given in general practice. A lack of specialized knowledge and therapeutical directives based on that, leaves the patient vulnerable in early stages for developing psychiatric symptoms [20] .
We developed an educational workshop (2 x 90 minutes) entitled ‘Control Over Tinnitus’ (COT) based on our earlier published neuropsychological theory of tinnitus mechanisms [21] , which can be applied effectively in the early stages of tinnitus. The workshop can be given to a group as well as to the individual patient, preferably within three months after the onset of symptoms (period of adjustment).
The primary aim of this evaluation is to investigate whether COT leads to reduction of tinnitus related disabilities in new tinnitus patients. We hypothesize that COT does not effect tinnitus severity, but that it will reduce tinnitus related problems as measured by the Tinnitus Handicap Inventory (THI) [22] .
Materials and Methods
Procedure
Participants in the current evaluation were new consecutive patients who, because of tinnitus, consulted the Ear, Nose and Throat (ENT) outpatient clinic of the Erasmus University Hospital Rotterdam, the Netherlands. They were each clinically examined by an ENT doctor and audiometrically assessed as part of the diagnostic protocol. To all patients who were diagnosed with subjective tinnitus, COT was offered by verbal introduction and an information booklet about the workshop. Having tinnitus was the only inclusion criterium. Exclusion criteria were: clinical suspicion of dementia, drug abuse or psychosis. For those patients and patients who were not willing to participate in a group, COT was offered individually. Participants of individual COT are excluded from this evaluation.
COT was organized as a monthly standard education for a heterogenous group. In a written introductory letter before the start of COT, it was explained to the participants that filling out questionnaires was not a part of the education and that helping to evaluate the workshop was on a voluntary basis. Questionnaires were asked to be filled out before the actual beginning of the education. New COT group meetings were held every two weeks and consisted of 10-15 new patients. In the information booklet which was given at invitation, their spouse or relative was invited to join. In general, this led to an average group size of 20-30 people, with half of them being a tinnitus patient. The maximum waiting time for participation in COT was one month.
Measures
Educational level was assessed by the level of highest attended school, categorized into 3 groups (low, middle, high). The impact of tinnitus in daily living was assessed with the THI at T1. The primay outcome was the reduction in score of the THI at T2. The original THI has a hightest-retest reliability [23] . The maximum total score is 100. A higher total score indicates a worse outcome, reflecting the overall self-report of unwellbeing and social impairment because of tinnitus. In addition to the use of the total score, subscale scores were evaluated. The subscales of the THI reflect three domains: functional limitations, emotional responses and catastrophic responses [24] . Answering possibilities were ‘yes’ (scored with 4 points), ‘sometimes’ (2 points) or ‘no’ (0 points).
We additionally asked: (1) how frequently tinnitus was heard, using a five point scale, ranging from continuous to less than 4 times a month (‘incidental’), (2) whether they had been receiving other treatments for tinnitus after their participation in COT (answering possibilities were ‘no’,’medication’, ‘psychological counseling’, ‘fysiotherapy, acupuncture or other alternative therapy’ and ‘fitting hearing aids’) and (3) whether they personally felt that the education had been of significant help to them, to which they could answer ‘yes’ or ‘no’.
The THI and answers to the additional questions were assessed before the actual start of COT (T0), six weeks after COT (T1) and again twelve months (T2) after COT (T1 and T2 by postal survey).
Intervention
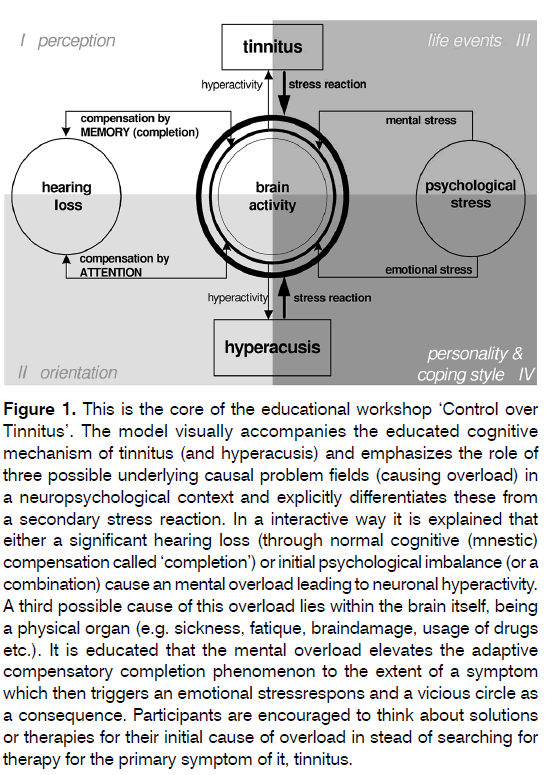
The intervention consisted of 2 consecutive educational, interactive sessions of 90 minutes, separated by a 60 minutes break. The cognitive mechanism of tinnitus was explained using a visual representation of the neuropsychological model (Figure 1) proposed byus in 2010 [21] . In the first part, called ‘Control over Causes”, the preservation of auditive streams were educated by explaining cognitive mechanisms using memory and attention and their role in auditive perception. Mental processes were emphasized. Then a parallel was made with effects on mental processes accompanying psychological and psychosocial dysfunctioning without significant hearing loss.
Figure 1: This is the core of the educational workshop ‘Control over Tinnitus’. The model visually accompanies the educated cognitive mechanism of tinnitus (and hyperacusis) and emphasizes the role of three possible underlying causal problem fields (causing overload) in a neuropsychological context and explicitly differentiates these from a secondary stress reaction. In a interactive way it is explained that either a significant hearing loss (through normal cognitive (mnestic) compensation called ‘completion’) or initial psychological imbalance (or a combination) cause an mental overload leading to neuronal hyperactivity. A third possible cause of this overload lies within the brain itself, being a physical organ (e.g. sickness, fatique, braindamage, usage of drugs etc.). It is educated that the mental overload elevates the adaptive compensatory completion phenomenon to the extent of a symptom which then triggers an emotional stressrespons and a vicious circle as a consequence. Participants are encouraged to think about solutions or therapies for their initial cause of overload in stead of searching for therapy for the primary symptom of it, tinnitus.
The suggestion was made that tinnitus is an auditory symptom of neurocognitive overload, rather than a mere symptom of hearing loss. The visual model was used to strengthen the insight in different possible causes of neurocognitive hyperactivity. It was then pointed out that tinnitus is a consequence of overload as a result of a foregoing stressor, rather than an idiopatic phenomenon or disease [21] .
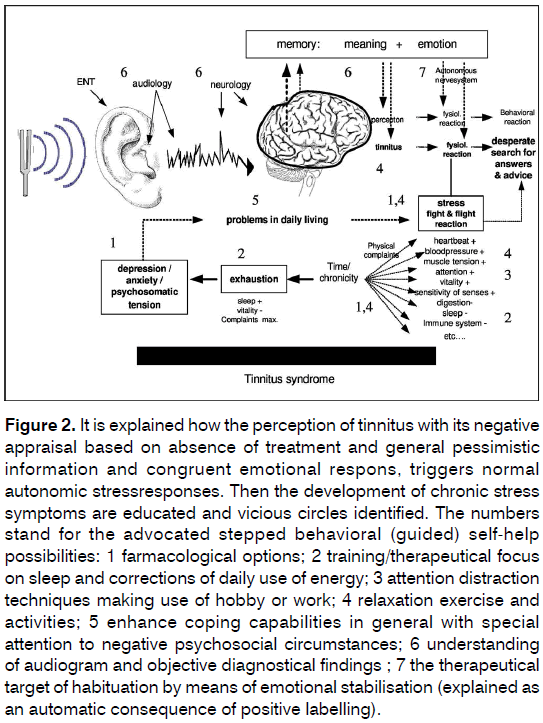
In the second part, called ‘Control Over Consequences’, reactive stress mechanisms were explained, pointing out a transition by time from active fight or flight reaction to a passive, ‘burned out syndrome’, consisting of emotional, physical and functional consequences of chronic stress from tinnitus. Vicious circles were identified. Again the education was build upon and accompanied by a visually presented schema (Figure 2). In this part of the workshop it was stated that the absence of soothing answers to the patients core-questions in an early stage leading tot maladaptive coping, may have lead to a negative appraisal of the perception and consequently to chronic stress reactions [25] .
Figure 2. It is explained how the perception of tinnitus with its negative appraisal based on absence of treatment and general pessimistic information and congruent emotional respons, triggers normal autonomic stressresponses. Then the development of chronic stress symptoms are educated and vicious circles identified. The numbers stand for the advocated stepped behavioral (guided) self-help possibilities: 1 farmacological options; 2 training/therapeutical focus on sleep and corrections of daily use of energy; 3 attention distraction techniques making use of hobby or work; 4 relaxation exercise and activities; 5 enhance coping capabilities in general with special attention to negative psychosocial circumstances; 6 understanding of audiogram and objective diagnostical findings ; 7 the therapeutical target of habituation by means of emotional stabilisation (explained as an automatic consequence of positive labelling).
Throughout the education the psychological and somatic changes, symptoms and behaviors were ‘normalized’ by placing them in connection with an understandable feeling of threat. The education concluded with a step by step identification of optional self-help interventions for preventing or reducing symptoms of chronic stress, thus offering the patients active directions to overcome feelings of powerlessness and to preserve (or regain) psychological-somatic strength.
Statistics
Population characteristics were described by means and percentages. Outcome variables were tested for normal distribution. When the data was normally distributed, t-tests and means with standard deviations (SD) were used. When the data was not normally distributed non parametric tests and medians were used.
To compare the outcome parameters before and after the intervention we used paired statistics. The emotional subscale of the THI was not normally distributed and thus the nonparametric related sample Wilcoxon signed rank test was used to analyze these data. Patients who did not fill in all items of all three consecutive THI questionnaires were excluded from analysis with THI scores. Data were analyzed using IBM SPSS version 21.
Results
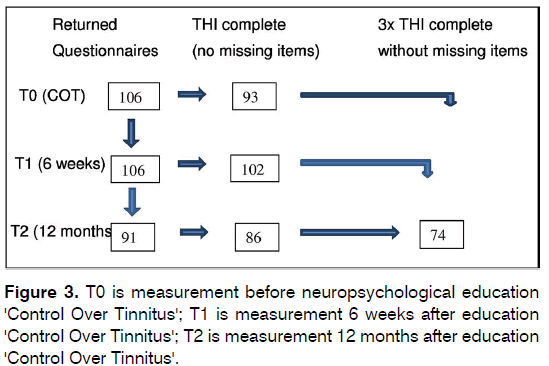
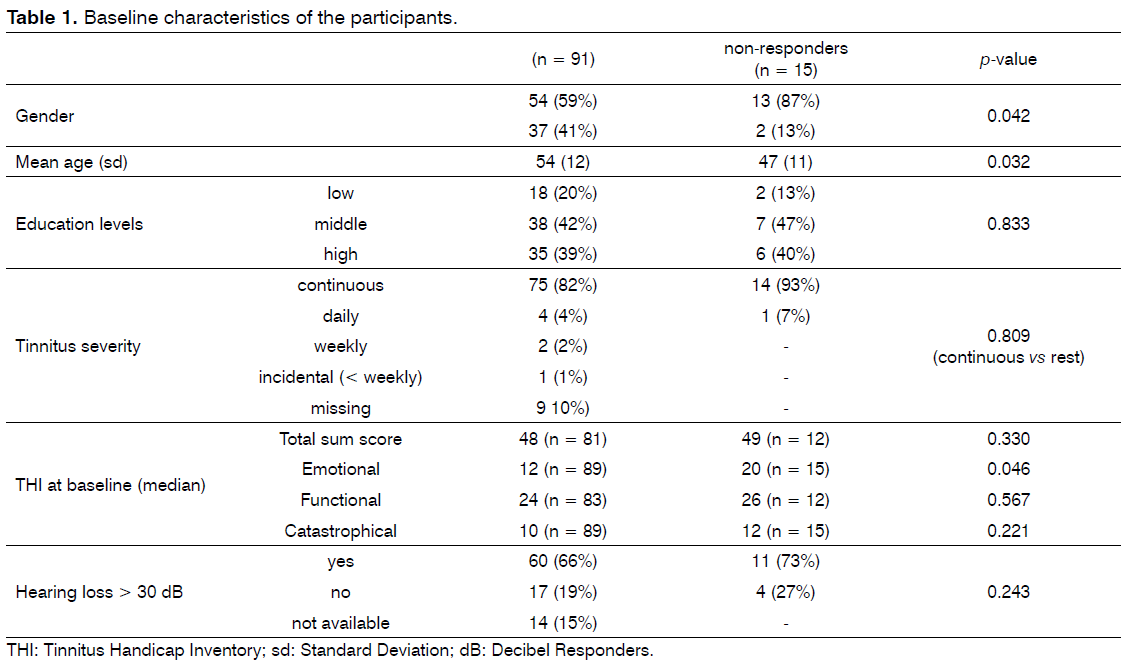
At baseline (T0), 106 participants finished the COT education and all were assessed with the THI. Six weeks (T1) and twelve months later (T2) they all received the THI again. After 12 months the THI was returned by 91 patients (86%). Figure 3 shows the flow chart of the participants. Characteristics of the 91 responders and 15 non-responders are presented in Table 1. These groups differed statistically with respect to gender, age and the emotional subscale of the THI. Ninety-six percent of the participants reported to have had audiometry. Seventy-four patients did answer all THI questions at all 3 assessments (‘complete responders’) and were included for analysis with THI scores (Figure 3).
The baseline characteristics of these 74 patients were compared with the 32 patients with missing data. There were no statistical significant differences in age, gender, education levels, tinnitus frequency (severity) and THI scores.
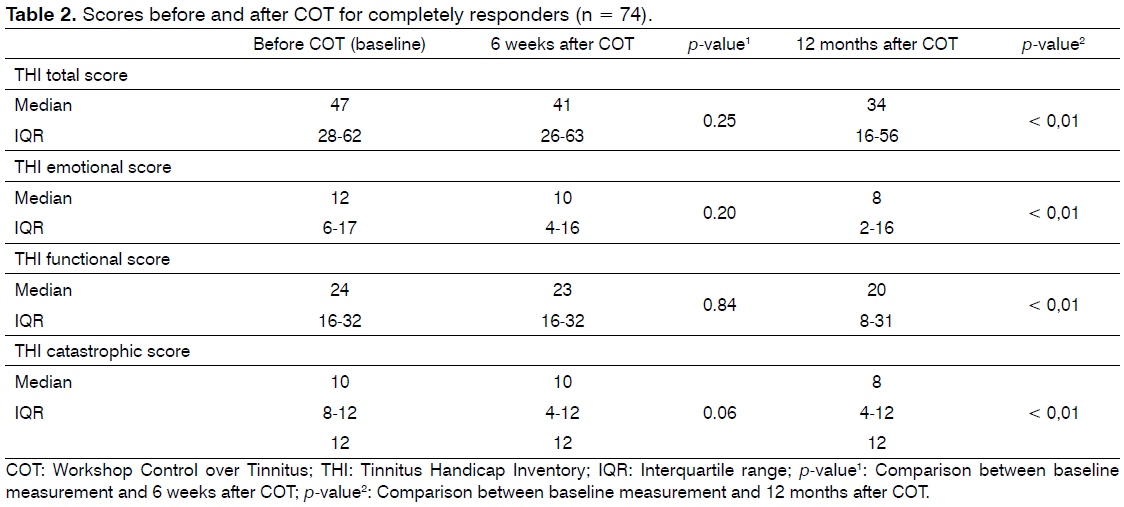
The scores on the THI and its subscales at baseline, after 6 weeks and 12 months are presented in Table 2. At six weeks, there was a trend for a decrease in catastrofic reactions (p = 0.06). Twelve months post intervention a significant decrease in THI total score and all subscales (the primary outcome variable) was observed (all p values ≤ 0.01).
Before COT, 92% of the participants reported continuous tinnitus, compared with 91% six weeks and 88% 12 months after COT. None of the patients had received a tinnitus focused therapy before COT and all patients had only received basic information by the general practioner or on the internet before referral. 65% of the 91 responders received no other treatment after COT, whereas 11% started psychological counseling, 9% received one or two hearing aids, 4% received physiotherapy, 4% used medication, 2% started Cognitive Behavioral Therapy (CBT) and 4% tried alternative treatments.
At 12 months, all 91 participants answered the question whether they personally felt COT had been helpful for them. Fifty-four of them (54%) answered positive on that question. Forty-three percent (23/54) of them received an additional intervention elsewhere after COT, whereas this was 24% (X2= 3.21; p = 0.07) in the participants who did not feel COT had been helpful. There were no statistical significant differences between participants rating the COT as helpful or not, with respect to THI scores or tinnitus severity.
Conclusion
The purpose of this evaluation was to investigate whether neuropsychological psychoeducation (workshop Control over Tinnitus), which was based on our earlier published model [21] , as a first step intervention, would decrease the tinnitus related emotional and functional impairments of tinnitus patients, despite ongoing tinnitus. Our findings support that hypothesis; the majority of participants considered additional therapy unnecessary despite a natural course of tinnituspatients towards varied but significant suffering [5] .
We found that at 12 months after COT the score on the Tinnitus Handicap Inventory was significantly reduced compared to baseline, despite ongoing tinnitus. A trend was already seen in the reduction of catastrophic thinking 6 weeks after COT, indicating reassurance. The significant decrease in reported impairments (from a mean of 45 to 38 points) in one year after only 180 minutes of standardized neuropsychological education can be considered as fairly good in comparison with extensive CBT [16] .
The decrease in the THI scores in the multi-stepped care treatment of Cima et al. [16] covering several elements (including education) was from a mean of 39 to 26. Which of the different elements of that therapy contributed to the improvements was unknown. Phillips et al. [9] reported a decrease of 18 points on THI score after Tinnitus Retraining Therapy.
Although there was no control group, making it impossible to draw conclusions from our evaluation, the reduction in the tinnitus related impairments seems to suggest that a progressive decline of well being due to tinnitus could be prevented by neuropsychological psychoeduction when given within the first three months of tinnitus.
Other factors may have accounted for the improvement of well being in our population. First of all, additive treatments may explain the improvement. However, most of the patients chose not to use other therapies. This may indicate reassurance, which makes this a less likely explanation of our results. In fact, one of the behavioral self-help directives of COT is to seek and select further therapy if necessary on the basis of insight instead of panic.
Second, it could have been the case that the majority of participants were simply not prone to develop psychological imbalance, for the determinants of a deviant course in wellbeing are insufficiently clear.
Thirdly, natural habituation of tinnitus regardless the education may explain the improvements observed in the current evaluation. In our opinion, this is unlikely because the course of an individual’s state of well being in bothersome tinnitus without further specialized therapy, typically progresses towards significant psychological suffering [5] . Furthermore, the THI score represents a subjective judgment of well being and is therefore dependent on psychological health and satisfaction about the offered care and feelings of being understood by health care professionals.
Tyler et al. [26] as well as Henry et al. [27] have suggested that every clinical tinnitus management program should consist of education. To this end, they advised educational counselling and suggested that additional therapy by psychologists or other mental health care professionals would be required only in cases of psychiatric comorbidity. We tend to agree with them as long as an educational protocol like COT takes place as early as possible in order to emotionally stabilize the tinnituspatient and reduce the risk of psychopathological development.
In our opinion, education should not be used only as an introduction for a tinnitus therapy but as a first step, stand alone intervention with a therapeutic purpose of its own. In this sense, we suggest that the educational emphasis should be directed towards emotional stability, self-help, or therapeutic compliance, while addressing self-awareness and one’s own capacity to effect change in circumstances. Fot that reason the education should be standardized, like the neuropsychological education of COT. In that way it can take on the role of a first step in a stepped care approach in which every single step should be potentially the last step.
Randomized and blind studies using different educational paradigms and a control group would be necessary in order to be able to draw conclusions. Additionally, longitudinal research of determinants for the development of psychiatric comorbidity because of tinnitus is needed to maximize the efficiency of specialized education in general health care. As the patients in this evaluation were recruited from a tertiary ENT department, results cannot plainly be applied to other populations.
We conclude that the neuropsychological educational protocol COT may be a sufficient first step intervention for new tinnitus sufferers, helping them to cope with tinnitus. This is relevant as regards to treatment efficiency and prevention of psychiatric disorders.
References
- Heller AJ. Classification and epidemiology of tinnitus. OtolaryngolClin North Am. 2003;36(2):239-48.
- Geocze L, Mucci S, Abranches DC, Marco MA, Penido NO. Systematic review on the evidences of an association between tinnitus and depression. Braz J Otorhinolaryngol. 2013;79(1):106-11.
- Gomaa MA, Elmagd MH, Elbadry MM, Kader RM. Depression, Anxiety and Stress Scale in patients with tinnitus and hearing loss. Eur Arch Otorhinolaryngol. 2014;271(8):2177-84.
- Langguth B, Landgrebe M, Kleinjung T, Sand GP, Hajak G. Tinnitus and depression. World J Biol Psychiatry. 2011;12(7):489-500.
- Rubinstein B. Tinnitus and craniomandibular disorders--is there a link? Swed Dent J Suppl. 1993;95:1-46.
- Lindberg P, Lyttkens L, Melin L, Scott B. Tinnitus--incidence and handicap. ScandAudiol. 1984;13(4):287-91.
- Andersson G. Psychological aspects of tinnitus and the application of cognitive-behavioral therapy. ClinPsychol Rev. 2002;22(7):977-90.
- Konzag TA, Rübler D, Bandemer-Greulich U, Frommer J, Fikentscher E. [Psychological comorbidity in subacute and chronic tinnitus outpatients]. Z Psychosom Med Psychother. 2005;51(3):247-60.
- Jozefowicz-Korczynska M, Ciechomska EA, Pajor AM. Electronystagmography outcome and neuropsychological findings in tinnitus patients. Int Tinnitus J. 2005;11(1):54-7.
- Rossiter S. Stevens C, Walker G. Tinnitus and its effect on working memory and attention. J Speech Lang Hear Res. 2006;49(1):150-60.
- Nondahl DM, Cruickshanks KJ, Wiley TL, Klein R, Klein BE, Tweed TS. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am AcadAudiol. 2002;13(6):323-31.
- Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. Tinnitus: causes and clinical management. Lancet Neurol. 2013;12(9):920-30.
- Hoekstra CE, Rynja SP, van Zanten GA, Rovers MM. Anticonvulsants for tinnitus. Cochrane Database Syst Rev. 2011;(7):CD007960.
- Baldo P, Doree C, Lazzarini R, Molin P, McFerran DJ. Antidepressants for patients with tinnitus. Cochrane Database Syst Rev. 2006;(4):CD003853.
- Hoare DJ, Edmondson-Jones M, Sereda M, Akeroyd MA, Hall D. Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochrane Database Syst Rev. 2014;(1):CD010151.
- Cima RF, Maes IH, Joore MA, Scheyen DJ, El Refaie A, Baguley DM, et al. Specialised treatment based on cognitive behaviour therapy versus usual care for tinnitus: a randomised controlled trial. Lancet. 2012;379(9830):1951-9.
- Jastreboff PJ. Tinnitus retraining therapy. Prog Brain Res. 2007;166:415-23.
- Henry JA, Schechter MA, Zaugg TL, Griest S, Jastreboff PJ, Vernon JA, et al. Clinical trial to compare tinnitus masking and tinnitus retraining therapy. ActaOtolaryngol Suppl. 2006;(556):64-9.
- Phillips JS, McFerran D. Tinnitus Retraining Therapy (TRT) for tinnitus. Cochrane Database Syst Rev. 2010;(3):CD007330.
- Cima RF, Crombez G, Vlaeyen JW. Catastrophizing and fear of tinnitus predict quality of life in patients with chronic tinnitus. Ear Hear. 2011;32(5):634-41.
- Wagenaar O, Wieringa M, Verschuure H. A cognitive model of tinnitus and hyperacusis; a clinical tool for patient information, appeasement and assessment. Int Tinnitus J. 2010;16(1):66-72.
- Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122(2):143-8.
- Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am AcadAudiol. 1998;9(2):153-60.
- Baguley DM, Andersson G. Factor analysis of the Tinnitus Handicap Inventory. Am J Audiol. 2003;12(1):31-4.
- Budd RJ, Pugh R. Tinnitus coping style and its relationship to tinnitus severity and emotional distress. J Psychosom Res. 1996;41(4):327-35.
- Tyler RS Haskell GB, Gogel SA, Gehringer AK. Establishing a tinnitus clinic in your practice. Am J Audiol. 2008;17(1):25-37.
- Henry JA, Zaugg TL, Myers PJ, Kendall CJ, Turbin MB. Principles and application of educational counseling used in progressive audiologic tinnitus management. Noise Health. 2009;11(42):33-48.
References
1Dept. of Otolaryngology-Head and Neck Surgery, section Audiology - VU University Medical Center, EMGO+ Institute - Amsterdam - AC - Netherlands. E-mail: ovwagenaar@gmail.com / m.vandenbrink@erasmusmc.nl / c.mantingh@erasmusmc.nl / se.kramer@vumc.nl
2Old Age Department - Parnassia Psychiatry Institute - The Hague - AC - Netherlands. E-mail: r.kok@parnassia.nl
Institution: Parnassia Psychiatry Institute, The Hague, The Netherlands Erasmus Medical Center Rotterdam, Dept. of Otorhinolaryngology and Head and Neck Surgery, Rotterdam, The Netherlands VU University Medical Center, Dept. of Otolaryngology-Head and Neck Surgery, section Audiology, EMGO+ Institute, Amsterdam, The Netherlands.
Send correspondence to:
Olav Victor Gerald Wagenaar
Pres. Kennedylaan 15
2517 JK, The Hague, The Netherlands
Paper submitted to the RBCMS-SGP (Publishing Management System) on February 05, 2016; and accepted on April 26, 2016. cod. 222
Citation: Wagenaar OVG, Wieringa M, Mantingh L, Kramer SE, Kok R. Preliminary longitudinal results of neuropsychological education as first and sole intervention for new tinnitus patients. Int Tinnitus J. 2016; 20(1) : 11-17