The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 26, Issue 2 / December 2022
Research Article Pages:89-94
10.5935/0946-5448.20220011
Tinnitus Evaluation in Type 1 Diabetes Mellitus at Tertiary Hospital Malaysia
Authors: Ameen SA, Norasyikin AW, Noor Dina H, Fahrin Zara MN, Tyler R, Asma Abdullah
PDF
Abstract
Objectives: To determine the prevalence of tinnitus in Type 1 Diabetes Mellitus (T1DM) patients, to evaluate its severity and to correlate it with estimated Glomerular Filtration Rate (eGFR) as well as glycaemia control (HbA1c).
Material and Methods: We performed a questionnaire-based cross-sectional study at Hospital Canselor Tuanku Muhriz (HCTM) from a period of 15 months. A total of 133 T1DM patients who fulfilled our study’s criteria were subjected to otoscopy examination, tuning fork test and free field voice test. The mini-Tinnitus Questionnaire (TQ) was used to assess the severity of tinnitus. We were careful to categorize the perceived duration of tinnitus.
Results: The prevalence of tinnitus among T1DM patients was 24.1% (32/133 patients). Out of 32 patients, approximately 78.1% (25 patients) had a compensated level of tinnitus distress and the remaining 21.9% (7/32) had moderate tinnitus. The duration of tinnitus ranged from 2 seconds to 2 minutes, wh?ch was ringing and intermittent in nature. The HbA1c and estimated Glomerular Filtration Rate (eGFR) were higher in tinnitus compared to the non-tinnitus group. There was no significant correlation between the severity of tinnitus and HbA1c level or eGFR.
Conclusions: Our study concluded that tinnitus amongst T1DM patients was likely to be non-pathological in view of its short duration with minimal to no distress to the sufferers. An elevated HbA1c may increase the risk of develop?ng tinnitus.
Keywords: Tinnitus, Type 1 diabetes mellitus, Mini-tinnitus questionnaire, Estimated glomerular filtration rate
Introduction
Tinnitus is the perception of sound for which there is no acoustic source external to the head1. Dauman and Tyler proposed that pathologic tinnitus is head noise lasting at least 5 minutes that occurs more than once per week2. A distinction is often made between subjective and objective tinnitus3. Subjective tinnitus refers to an internal sound that is perceived only by the patient, whereas objective tinnitus is considered real noise that can be heard by the patient and the examiner4 Failure to treat chronic tinnitus may affect the patient’s psychology w?th varying severity.
Change in the cochlear inner hair cell ion channels (e.g. L-Type calcium, potassium and sodium channels) and receptor systems may predispose to tinnitus5-8. Other predisposing factors are aging, cochlear ablation, noise trauma and global brain activation secondary to tinnitusinducing agents e.g. salicylate8.
A study performed by Mousav? et al ?n 2021 revealed 26.4% of pat?ents w?th d?abetes suffered w?th t?nn?tus (n=250)4. They also d?scussed t?nn?tus prevalence ?n prev?ous reports of 19-65% amongst the general population. The National Study of Hearing in the UK (n=48,313) by Davis showed tinnitus prevalence of 10?1% amongst adults.5 An Asian population study conducted in Korea (n=19,290) revealed a prevalence of 20.7%6. Swain et al found that the prevalence amongst 240 diabetic patients was 29.1%7 Baharudin et al recorded a prevalence in Type 2 Diabetes Mellitus (T2DM) patients ?n University Kebangsaan Malaysia was of 9.1%8. Klagenberg et al reported prevalence amongst T1DM patients was as 13.3%9.
There are various conditions associated with tinnitus. Otological conditions are infectious (otitis media, labyrinthitis, mastoiditis), neoplastic (vestibular schwannoma, meningioma), labyrinthine (Meniere’s disease, vestibular vertigo, sensorineural hearing loss) amongst others (otosclerosis, presbycusis and noise exposure). Endocrine or metabolic conditions include diabetes mellitus, hypothyroidism, hyperinsulinemia and pregnancy. Neurological conditions include meningitis, migraine and multiple sclerosis. Other conditions are psychiatric (anxiety, depression, emotional trauma), ototoxic medications (diuretics, immunosuppressive drugs, non-stero?dal ant?-?nflammatory drugs (NSAIDS), corticosteroids), systemic lupus erythematosus (SLE), rheumatoid arthritis, hypertension, head injury and temporo-mandibular joint disorders10.
Materials and Methods
A questionnaire-based cross-sectional study was done over a period of 15 months at the Endocrine Clinic (Adult and Pediatric) and Primary Care Clinic Hospital Canselor Tuanku Muhriz (HCTM) follow?ng approval from local research and Ethics Committee. The study inclusion criteria included patients with T1DM diagnosed at HCTM with or without hypertension, and patients aged 12 to 50 years. The results of renal profile and HbA1c level were documented. Exclusion criteria included patients
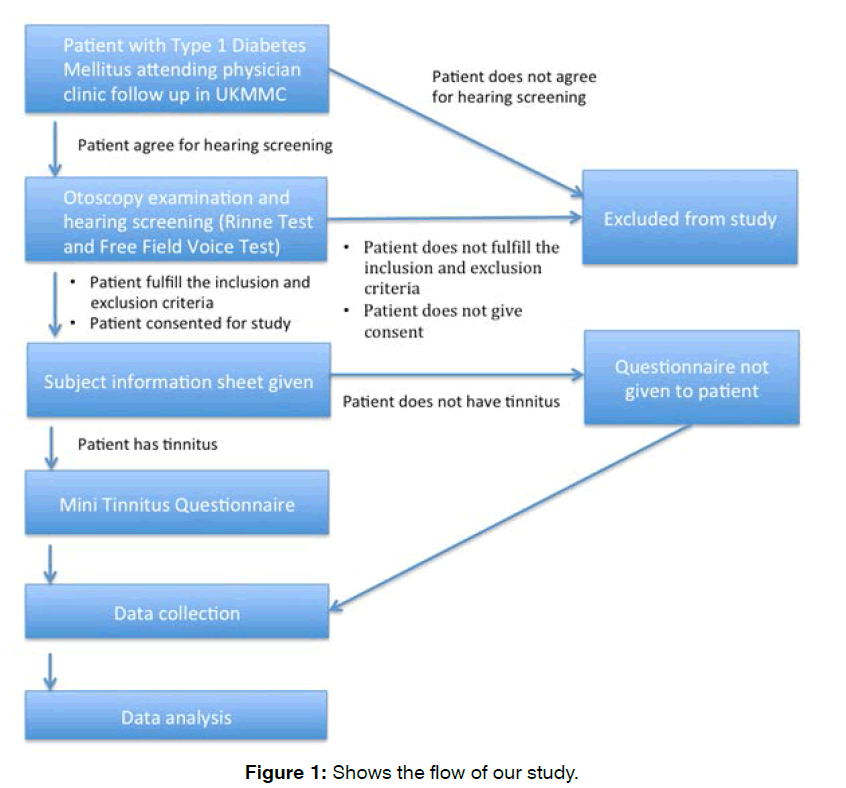
Our study patients underwent a hearing assessment to rule out hearing loss as part of the exclusion criteria. Th?s was followed by an otoscopy examination, tun?ng fork test, as well as a Free Field Voice Test. Informed consent was obta?ned from patients who fulfilled the inclusion and exclusion criterias. Demographic data and other relevant information pertaining to the research was obtained via questionnaire. Patients with tinnitus were given the mini- TQ questionnaire. All ?ncomplete questionnaires resulted ?n pat?ent exclusion. The mini-tinnitus questionnaire is an abridged version of Tinnitus Questionnaire. Pat?ents were prov?ded w?th the m?n?-TQ ?n 2 languages, wh?ch was randomly d?str?buted amongst pat?ents. All the data obtained will be collected and analysed using SPSS software. Correlations between these variables were also assessed using the Spearman Correlation test. Statistic significance was set at p value of less than 0.05 (p<0.05). Chi-Square test was used to assess variable in groups (Figure 1).
Figure 1: Shows the flow of our study.
Results
A total of 133 patients were recruited. Table 1 shows the epidemiology of the patients. Of the 133 patients, 45.9% (61) of them were males and 54.1% (72) were female. Most of the participants (48.1%) are from the ‘21-30’ age group. The majority of the participants were Chinese (54.1%), followed by Malay (35.3%), Indian (8.3%) and Punjabi (2.3%).
| Epidemiology of Type 1 diabetes Mellitus patients | |
|---|---|
| AGE | No (%) |
| 12-20 years old | 46 (34.6) |
| 21-30 years old | 64 (48.1) |
| 31-40 years old | 15 (11.3) |
| 41-50 years old | 8 (6.0) |
| GENDER | |
| Male | 61 (45.9) |
| Female | 72 (54.1) |
| RACE | |
| Malay | 47 (35.3) |
| Chinese | 72 (54.1) |
| Indian | 11 (8.3) |
| Others | 3 (2.3) |
Table 1: Shows the epidemiology of the patients.
The prevalence of tinnitus amongst T1DM patients in this study was 24.1% (32).
Table 2 shows the epidemiology and tinnitus characteristics in the tinnitus group. Most of the patients with tinnitus are from the ‘12-20’ years group. All of them have intermittent and ringing-type tinnitus. The majority of the patients (65.6%) had tinnitus for a duration of less than 10 seconds.
| Age Group | No (%) |
|---|---|
| 12-20 years old | 16 (50) |
| 21-30 years old | 13 (40.6) |
| 31-40 years old | 3 (9.3) |
| Gender | |
| Male | 20 (62.5) |
| Female | 12 (37.5) |
| Race | |
| Malay | 15 (46.9) |
| Chinese | 17 (53.1) |
| Tinnitus Localisation | |
| Right | 11 (34.4) |
| Left | 9 (28.1) |
| Both | 12 (37.5) |
| Tinnitus Character | |
| Intermittent | 32 (100) |
| Tinnitus noise type | |
| Ringing | 32 (100) |
| Tinnitus duration | |
| <10secs | 21 (65.6) |
| 10-59secs | 10 (31.3) |
| 60secs-30secs | 1 (3.1) |
Table 2: Shows the epidemiology and tinnitus characteristics in the tinnitus group.
Table 3 shows the co-morbid?t?es amongst the tinnitus group of patients. Only two (6%) had hyperlipidemia, one (3%) had a history of repaired Patent Ductus Arteriosus (PDA), and 2 (6%) had hypothyroidism and was on thyroxine supplementat?on.
| Comorbid | n | % |
|---|---|---|
| Hypertension | 1 | 3.1 |
| Hyperlipidaemia | 2 | 6.2 |
| Heart disease (PDA) | 1 | 3.1 |
| Thyroid disease (hyperthyroidism) | 2 | 6.2 |
| Others (Allergic rhinitis, Asthma) | 2 | 6.2 |
Table 3: Shows the co-morbid?t?es amongst the tinnitus group of patients.
Table 4 shows the percentage of tinnitus across the age groups. Most of the participants with tinnitus belong to the ‘12-20’ age group (12.8%) with 17 participants, followed by ‘21-30’ age group (9%) with 12 participants and least was ?n the ‘31-40’ age group.
| Type 1 DM/ Age group |
Without tinnitus | With tinnitus | X2 | P-Value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| 12-20 | 29 | 21.8% | 17 | 12.8% | 7.845 | 0.049 |
| 21-30 | 52 | 39.1% | 12 | 9.0% | ||
| 31-40 | 12 | 9.0% | 3 | 2.3% | ||
| 41-50 | 8 | 6.0% | 0 | 0.0% | ||
| TOTAL | 101 (75.9%) | 32 (24.1%) | ||||
Table 4: Shows the percentage of tinnitus across the age groups.
Table 5 shows the severity of tinnitus based on the mini-TQ questionnaire amongst the tinnitus group of patients. The majority of patients (n=25, 78.1%) have a compensated level of tinnitus distress (no clinically relevant distress due to the tinnitus), whilst the others (n=7, 21.9%) have a tinnitus severity of moderate distress level. None of them were in the ‘severe distress’ or ‘most severe distress’ group.
| Mini TQ Severiti Index (n=32) | Frequency | Percent (%) |
|---|---|---|
| Compensated | 25 | 78.1 |
| Moderate distress | 7 | 21.9 |
| Severe distress | 0 | 0.0 |
| Most severe distress | 0 | 0.0 |
Table 5: Shows the severity of tinnitus based on the mini-TQ questionnaire amongst the tinnitus group of patients.
Table 6 compares the HbA1c level between tinnitus and non-tinnitus groups HbA1c level was statistically significantly higher ?n the t?nn?tus group compared to the group without tinnitus (U= 1112, p=0.008).
| HbAIC Mean ± SD |
Without tinnitus (n-101) 8.65 ± 1.86 |
With tinnitus (n=32) 9.87 ± 2.30 |
Mann-Whitney U test | ||
|---|---|---|---|---|---|
| U | Z | p-value | |||
| Mean rank | 62.01 | 82.75 | 1112.00 | -2.654 | 0.008 |
Table 6: compares the HbA1C level between tinnitus and non-tinnitus groups HbA1C level was statistically significantly higher ?n the t?nn?tus group compared to the group without tinnitus (U= 1112, p=0.008).
Table 7 shows correlation of HbA1c level with mini-TQ total score (tinnitus severity) amongst the tinnitus group of participants. The results shows that there is small negative correlation between HbA1c level and tinnitus severity, however, th?s ?s not stat?st?cally significant (p>0.05).
| Tinnitus Severity | HbAIC level | ||
|---|---|---|---|
| Tinnitus Severity | Pearson Correlation Sig. (2-tailed) N |
1 32 | -0.141 0.441 32 |
| Spearman Correlation coefficient sig. (2 tailed)N |
1 32 | -0.138 0.451 32 |
|
Table 7: shows correlation of HbA1C level with mini-TQ total score (tinnitus severity) amongst the tinnitus group of participants.
Table 8 shows correlation between eGFR with mini-TQ total score (tinnitus severity). The result shows that there is small negative correlation between them but the result is not stat?st?cally significant (p>0.05).
| Tinnitus Severity | GFR level | ||
|---|---|---|---|
| Tinnitus Severity | Pearson Correlation Sig. (2-tailed) N |
1 32 | -0.141 0.441 32 |
| Spearman Correlation coefficient sig. (2 tailed)N |
1 32 | -0.138 0.451 32 |
|
Table 8: Shows correlation between eGFR with mini-TQ total score (tinnitus severity).
Discussion
Tinnitus may cause substantial distress. It may man?fest as annoyance, anxiety, depression, lack of concentration and sleep disturbance11 Diabetic microangiopathies and neuropathy affects the sensory organs i.e. the auditory pathway, and may cause symptoms such as hearing loss, tinnitus and vertigo12 Tinnitus commonly precedes hearing loss, which is described as high frequency, sensorineural, and progressive13 In this study, the prevalence of tinnitus amongst T1DM is 24.1% (32/133). It is higher compared to a (13.3%) study done by Klagenberg et al9 One possible cause for a higher prevalence of tinnitus, may be due to the criteria of tinnitus chosen in this study, which was independent of the duration.
Tinnitus prevalence ?n the general populat?on increases with age and usually peaks at around 70 years of age, whereby the prevalence then starts to drop as age increases4,19. Our study showed a h?gher prevalence ?n the younger age group, albe?t young T1DM pat?ents. Most of the participants with tinnitus (56.3%) reported tinnitus for approximately 5 seconds, and it was ‘ringing’ and ‘intermittent’ in nature. The time between each tinnitus episode varied. In our opinion, patterns of tinnitus in this study are believed to be non-pathological due to the fact that the longest duration of tinnitus recorded lasted for only 2 minutes. The majority of the patients (n=25, 78.1%) have a compensated level of tinnitus distress (no clinically relevant distress due to the tinnitus), wh?lst the others (n=7, 21.9%) have tinnitus severity of moderate distress level. This shows that most T1DM pat?ents with tinnitus have mild tinnitus which rarely causes distress. This was assumed by the fact that none of the patients complained of tinnitus to physicians during their consultations.
A study in Taiwan showed that Chronic kidney Disease (CKD) increased the risk of develop?ng tinnitus14 A combination of factors resulting from CKD, including abnormal electrolytes, urea and creatinine levels, may lead to cochlear microcirculation dysfunction causing damage to the cochlear15 In this study, we found a negative correlation of eGFR with tinnitus severity, albe?t not statistically significant. This study also revealed that there is no significant correlation of HbA1c with tinnitus severity, supported by a study with the same conclusion amongst diabetes T2DM Table 2 patients16
HbA1c reflects the average glucose levels of the prev?ous 3 months. The prolonged hyperglycemic state may disturb bra?n and ?nner ear funct?on, which may lead to the reduced processing of complex sounds. Th?s may be a contr?but?ng factor to the occurrence of tinnitus and hearing impairment17-19 Srinivas found that the prevalence of sensorineural hearing loss is was high (>85%) amongst subjects with HbA1c of more than 8.18 HbA1c levels in patients with tinnitus was found to be significantly higher than those without tinnitus in this study.
Conclusion
The prevalence of tinnitus amongst T1DM patients in this study was 24.1%. Based on the mini-TQ, 78.1% (n=25) had a compensated level of tinnitus distress and 21.9% (n=7) had a tinnitus severity of moderate distress level. Causes of tinnitus in T1DM are multifactorial. Duration of tinnitus ranged from 2 seconds to 2 minutes, was ringing and intermittent in nature, and therefore, of non-pathological type. The group with tinnitus had a significantly higher level of HbA1c compared to those without tinnitus. There was no significant correlation found between the severity of tinnitus with HbA1c level and eGFR in our study.
Acknowledgements
We would like to thank Prof. Dr. Wu Loo Liang from the Pediatric Department of HCTM for her collaboration and input in this study.
References
- Henry JA, Dennis KC, Schechter MA. General review of tinnitus.
- Lockwood AH. Tinnitus. Neurologic clinics. 2005;23(3):893-900.
- Dauman R, Tyler RS. Some considerations on the classification of tinnitus. Aran, JM Tinnitus, 91: Proceedings of the Fourth International Tinnitus Seminar. 225-229.
- Mousavi SH, Sajadinejad B, Khorsandi S, Farhadi A. Diabetes Mellitus and Tinnitus: an Epidemiology Study. Maedica. 2021;16(4):580.
- Davis, A, El Rafaie, A. Epidemiology of tinnitus. In: Tyler RS, ed. Tinnitus handbook. San Diego, CA: Singular, Thomson Learning, 2000;1-23.
- Cho YS, Choi SH, Park KH, Park HJ, Kim JW, Moon IJ, et al. Prevalence of otolaryngologic diseases in South Korea: data from the Korea national health and nutrition examination survey 2008. Clinical and Experimental Otorhinolaryngol. 2010;3(4):183-93.
- Padhy RN. Incidence of hearing loss, tinnitus and vertigo among diabetes patients. Siriraj Med J. 2014;66(5).
- Baharudin AS, Kiat NC, Isahak NF, Xin TW, Zhaki FN, Rashid NA, et al. Prevalence of Tinnitus in Type II Diabetes Mellitus with or without Hypertension Patients in Universiti Kebangsaan Malaysia Medical Centre. Int Med J. 2017;24(5):398-401.
- Klagenberg KF, Zeigelboim BS, Jurkiewicz AL, Martins-Bassetto J. Vestibulocochlear manifestations in patients with type I diabetes mellitus. Revista Brasileira de Otorrinolaringologia. 2007;73:353-8.
- Baguley D, McFerran D, Hall D. Tinnitus. The Lancet. 2013;382(9904):1600-7.
- Gopinath B, McMahon CM, Rochtchina E, Karpa MJ, Mitchell P. Risk factors and impacts of incident tinnitus in older adults. Ann of Epidemiol. 2010;20(2):129-35.
- Hadi HA, Al Suwaidi J. Endothelial dysfunction in diabetes mellitus. Vascular Health and Risk Management. 2007;3(6):853.
- Schalkwijk CG, Stehouwer CD. Vascular complications in diabetes mellitus: the role of endothelial dysfunction. Clin Sci. 2005;109(2):143-59.
- Shih CP, Lin HC, Chung CH, Hsiao PJ, Wang CH, Lee JC, ET AL. Increased risk of tinnitus in patients with chronic kidney disease: A nationwide, population-based cohort study. PLoS One. 2017;12(8):e0183192.
- Shih CP, Lin HC, Chung CH, Hsiao PJ, Wang CH, Lee JC, et al. Increased risk of tinnitus in patients with chronic kidney disease: A nationwide, population-based cohort study. PLoS One. 2017;12(8):e0183192.
- Somogyi A, Rosta K, Vaszi T. Hearing impairment and tinnitus in patients with type 2 diabetes. Orvosi Hetilap. 2013;154(10):363-8.
- Taneja N. Tinnitus, hearing impairment and diabetes: A mini-review. Otolaryngol Open J. 2017;SE(5): S6-S9.
- Srinivas CV, Shyamala V, Shiva Kumar BR. Clinical study to evaluate the association between sensorineural hearing loss and diabetes mellitus in poorly controlled patients whose HbA1c> 8. Indian J of Otolaryngol and Head & Neck Surg. 2016;68(2):191-5.
- Park KH, Lee SH, Koo JW, Park HY, Lee KY, Choi YS, et al. Prevalence and associated factors of tinnitus: data from the Korean National Health and Nutrition Examination Survey 2009–2011. J Epidemiol. 2014:JE20140024.
1Department of Otorhinolaryngology, University Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
2Department of Medicine, University Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
3Centre for Ear, Hearing and Speech (Institute-HEARS), Faculty of Health Sciences
4Department of Otolaryngology Head and Neck Surgery, Department of Communication Sciences and Disorders, The University of Iowa, Iowa City, United States.
Send correspondence to:
Asma Abdullah
Department of Otorhinolaryngology, University Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia, Kuala Lumpur, Malaysia. Tel: 03-9145 6599, Email: asmappukm@gmail.com
Paper submitted on July 26, 2022; and Accepted on August 17, 2022)
Citation: Ameen SA, Norasyikin AW, Noor Dina H, Fahrin Zara M N, Tyler R., Asma Abdullah Tinnitus Evaluation in Type 1 Diabetes Mellitus at Tertiary Hospital Malaysia. Int Tinnitus J. 2022;26(2):89-94.